By Leah Lawrence
Posted: June 2018
The use of trimodality therapy—the combination of chemoradiotherapy followed by surgery—remains controversial for patients with locally advanced cN2-N3 NSCLC.
According to the National Comprehensive Cancer Network guidelines, definitive chemoradiation therapy is the standard of care for the majority of patients with stage III NSCLC, and trimodality treatment is used only in selected patients with minimal N2 disease.
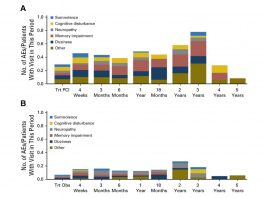
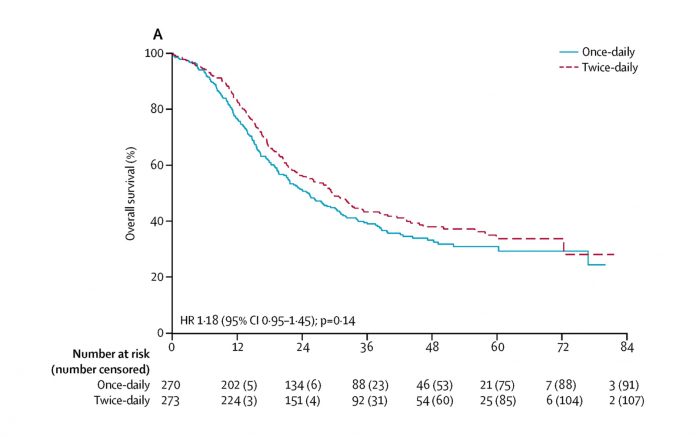
Results of the Intergroup 0139 study, one of the first randomized studies of concurrent chemoradiotherapy and trimodality approaches, showed that the 5-year progression-free survival was improved in patients who underwent trimodality treatment compared with bimodality therapy alone (hazard ratio = 0.77; 95% CI[0.62, 0.96]); however, this benefit did not translate into an overall survival advantage.1
“In a subset analysis of the study, they showed that patients who underwent a lobectomy did have a survival benefit with trimodality treatment, but this was an unplanned analysis,” said Melissa A.L. Vyfhuis, MD, PhD, of the University of Maryland Medical Center.
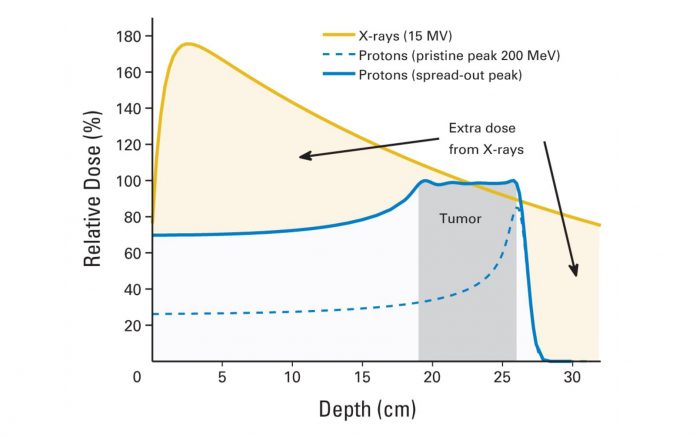
The lack of overall survival benefit may have, in part, been due to the trial’s high mortality rate seen with pneumonectomies. Furthermore, in the trial, they used a lower radiation dose of 45 Gy prior to surgical resection to offset the chance of an increase risk in morbidity or mortality associated with higher doses, according to Dr. Vyfhuis. “In the setting of stage III disease, we now know that [45 Gy] is not sufficient for cure,” Dr. Vyfhuis said. Practically speaking, if the tumor is deemed not resectable after such a low dose of radiation, then the patient would have to go back and receive additional radiation therapy, but now having sustained a significant break (typically 1 to 2 weeks) in their radiation treatments, which could affect clinical outcomes.
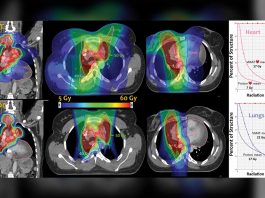
According to Dr. Vyfhuis, at the University of Maryland, she and her colleagues give a definitive dose of radiation (≥ 60 Gy) with concurrent chemotherapy, even if a patient was scheduled to undergo surgery; however, she acknowledged that not a lot of institutions routinely offer this dose as part of trimodality therapy.
“At University of Maryland, our surgeons have extensive experience operating on patients after the administration of a definitive dose (≥ 60 Gy) of radiation. This has resulted in low rates of postsurgical morbidity and mortality, especially for those patients undergoing a lobectomy,” Dr. Vyfhuis explained.
Dr. Vyfhuis and colleagues recently published the results of a study that showed that trimodality treatment with a radiation dose of at least 60 Gy significantly improved survival and freedom from recurrence in patients with locally advanced NSCLC.2
 In our experience, patients who attain mediastinal nodal clearance after neoadjuvant chemoradiation, no matter how bulky or extensive the disease was initially, can benefit from trimodality therapy.
In our experience, patients who attain mediastinal nodal clearance after neoadjuvant chemoradiation, no matter how bulky or extensive the disease was initially, can benefit from trimodality therapy.
–Melissa A.L. Vyfhuis, MD, PhD
The retrospective analysis included data from 355 consecutive patients with locally advanced NSCLC treated with curative intent between January 2000 and December 2013. Those patients who received trimodality therapy had a significantly longer median survival compared with patients with either unplanned or planned bimodality treatment (59.9 vs. 20.1 vs. 17.3 months, respectively; p < 0.001). The addition of surgery also benefited patients with stage IIIb (p < 0.001) and N3 (p = 0.010) nodal disease, especially when mediastinal nodal clearance was achieved.
“A median survival of approximately 60 months is essentially unheard of in stage III disease,” Dr. Vyfhuis said, adding that as a retrospective study some selection bias may be present. “In our experience, patients who attain mediastinal nodal clearance after neoadjuvant chemoradiation, no matter how bulky or extensive the disease was initially, can benefit from trimodality therapy.”
How Does It Fit?
The current standard of care for patients with stage III NSCLC may soon be changing however, according to Martin J. Edelman, MD, chair of the department of hematology/oncology at Fox Chase Cancer Center, and formerly of the University of Maryland Greenebaum Comprehensive Cancer Center.
In 2017, results of the phase III PACIFIC trial showed that the administration of the anti–PD-1 antibody durvalumab after definitive chemoradiotherapy more than tripled the median progression-free survival compared with chemoradiotherapy followed by placebo (16.8 vs. 5.6 months; p < 0.001).3 The results were presented at the 2017 European Society for Medical Oncology Congress and published in The New England Journal of Medicine. Based on these results, the standard of care today for a patient with locally advanced NSCLC is chemoradiotherapy followed by immunotherapy, according to Dr. Edelman.
“The trial was done predominantly in Europe, a little bit differently than we might have done it in the United States, but results were impressive,” Dr. Edelman said. “We do not yet have overall survival results, but I would be surprised if they do not echo the substantial improvements in progression-free survival that was published.”
The integration of immunotherapy into treatment regimens for patients with stage III disease only further complicates matters. Many questions remain, Dr. Edelman said.
“We still do not know the optimal chemotherapy regimen to use in combination with radiation,” Dr. Edelman said.“We feel following chemoradiotherapy with immunotherapy is good, but do not know if immunotherapy should follow immediately.”

Trimodality care should be restricted to experienced institutions that have high volume and an experienced multimodality team.
–Martin J. Edelman, MD
With so many questions remaining about bimodality therapy, it is hard to know where surgery would fit in.
According to Dr. Edelman, an ideal candidate for trimodality treatment would be someone who is relatively fit, with an otherwise good performance status. Ideally, the patient would require a lobectomy and not a pneumonectomy or another type of complex procedure, and would have mediastinal nodal disease that is not bulky. “Those patients in the correct hands should have a very low operative mortality,” Dr. Edelman said. However, outside of these situations, the standard of care remains bimodality therapy, he added.
“The problem with trimodality studies is how one integrates all three modes of treatment is very difficult, and each study has to be evaluated by itself because no two of them held all features constant,” Dr. Edelman explained.
When he was at the University of Maryland, using a radiation dose of 60 Gy with chemotherapy was feasible. If a patient did not go on to surgery, this meant that the proper definitive radiation dose had been administered. However, this approach may not be feasible in all institutions.
“Trimodality care should be restricted to experienced institutions that have high volume and an experienced multimodality team,” Dr. Edelman said. “Patients who are felt to be suitable for this treatment should be selected prior to initiation of any treatment.” ✦
References:
1. Albain KS, Swann RS, Rusch VR, et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small cell lung cancer. Lancet. 2009;374:379-386.
2. Vyfh uis MAL, Bhooshan N, Burrows WM, et al. Oncological outcomes from trimodality therapy receiving definitive doses of neoadjuvant chemoradiation (≥60 Gy) and factors influencing consideration for surgery in stage III non-small cell lung cancer. Adv Radiat Oncol. 2017;2:259-269.
3. Antonio SJ, Villegas, Daniel D, et al. Durvalumab after chemoradiotherapy in stage III non-small cell lung cancer. N Engl J Med. 2017;377:1919-1929.