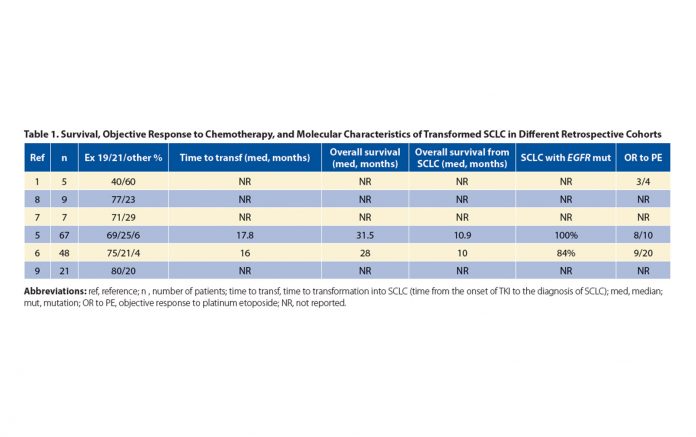
Abbreviations: ref, reference; n , number of patients; time to transf, time to transformation into SCLC (time from the onset of TKI to the diagnosis of SCLC); med, median; mut, mutation; OR to PE, objective response to platinum etoposide; NR, not reported.
By Denis Moro-Sibilot, MD, MSc
Posted: April 16, 2020

EGFR tyrosine kinase inhibitors (TKIs) are the standard of care for mutated EGFR NSCLC. Today, one of the burning questions is whether to select the most recent third-generation agent or to combine a first- or second-generation TKI with chemotherapy or antiangiogenic agents and reserve third generation inhibitors for patients who exhibit acquired resistance due to T790 mutations. Regardless of the first-line treatment chosen, resistance is, unfortunately, a nearly universal occurrence. The primary mechanism of resistance to first- and second-generation TKIs is represented by the appearance of the secondary resistance mutation T790M. This occurs approximately 50% to 60% of the time after treatment with first or second generation TKIs, but is extremely rare after treatment with osimertinib in the first-line setting. Among other mechanisms, transformation into SCLC is a relatively uncommon event, but it occurs regardless of the generation of TKI used, including osimertinib. SCLC transformation occurs in 3% to 10% of EGFR TKI‒resistant cases1,2; however, this incidence is possibly underestimated due to the absence of or inability to re-biopsy at the time of progression.3,4 Moreover, the simplicity of the analysis of circulating tumor DNA often limits the decision to re-biopsy, which is more complex to organize. Liquid biopsies obviously do not allow the diagnosis of SCLC transformation, which requires tissue.
Transformation to SCLC may occur at any time during the course of the disease, from the first few months to several years after the diagnosis of metastatic EGFR mt (+) NSCLC, but the average transformation time is approximately 13 to 18 months after the start of TKI treatment.5,6 Although these tumors have the usual histologic criteria of small cell carcinomas such as neuroendocrine differentiation, they differ from conventional SCLCs in that they occur in non-smokers or light smokers and frequently retain the original EGFR mutation, which is virtually never seen in de novo SCLC. More than two-thirds of SCLC transformations were observed in patients with EGFR exon 19 mutations (Table 1), whereas T790M resistance mutation is rarely observed in transformed SCLCs, even if it was present in the patient’s previous specimens, suggesting that this mutation may appear in a clone that is distinct from the clone that transforms to SCLC.
Losses of P53 and RB1 with inactivation of the two key alleles were identified in a majority of transformed SCLCs. A recent study compared 43 patients with the triple mutation (EGFR, P53, and RB1) to 142 controls with an EGFR mutation and wild-type P53 and RB1. Seven cases of SCLC were observed, all carrying the triple mutation, though only 18% of the triple mutants transformed, which shows that the P53 and RB1 mutations are necessary, but not sufficient, for transformation into SCLC.7 In sharp contrast, no transformation to SCLC was noted among patients whose tumors harbored the EGFR mutations alone.
Treatment Options: More Data Needed
The appearance of brain metastases is a frequent event, observed in two-thirds of patients during the evolution of SCLC.5 As with conventional SCLCs, retrospective data show sensitivity to standard chemotherapy combining etoposide and cisplatin (Table 1); other agents such as taxanes are also active.5 The continuation of TKI with chemotherapy is reported in a few retrospective cases; however, the value of such an association has not been demonstrated by clinical studies.
Immunotherapy, which is disappointing in mutated EGFR tumors, is also disappointing in these transformed tumors.5,10 As with mutated EGFR tumors, checkpoint inhibitors have had only limited activity in this setting. Based on the recent positive results of the CASPIAN and IMpower133 trials, the combination of etoposide and platinum with either durvalumab or atezolizumab may emerge, but it should be noted that neither trial included patients with transformed SCLC. Clinical trials in this group of patients are desirable, even if the relative rarity of these transformations will make it difficult to carry out such trials. After transformation, clinical behavior mimics the behavior of “classic SCLCs,” with a median overall survival of approximately 10 to 11 months, which confirms the poor prognosis of these transformed SCLCs. ✦
About the Author: Dr. Moro-Sibilot is with the Thoracic Oncology Unit, CHU Grenoble-Alpes, Grenoble, France.
References:
1. Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;23;3(75):75ra26.
2. Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res. 2013;19(8):2240-2247.
3. Bosc C, Ferretti GR, Cadranel J, et al. Rebiopsy during disease progression in patients treated by TKI for oncogene-addicted NSCLC. Target Oncol. 2015;10(2):247-253.
4. Redig AJ, Costa DB, Taibi M, et al. Prospective Study of Repeated Biopsy Feasibility and Acquired Resistance at Disease Progression in Patients With Advanced EGFR Mutant Lung Cancer Treated With Erlotinib in a Phase 2 Trial. JAMA Oncol. 2016;2(9):1240-1242.
5. Marcoux N, Gettinger SN, O’Kane G, et al. EGFR-Mutant Adenocarcinomas That Transform to Small-Cell Lung Cancer and Other Neuroendocrine Carcinomas: Clinical Outcomes. J Clin Oncol. 2019;37(4):278-285.
6. Ferrer L, Giaj Levra M, Brevet M, et al. A Brief Report of Transformation from NSCLC to SCLC: Molecular and Th erapeutic Characteristics. J Thorac Oncol. 2019;14(1):130-134.
7. Offin M, Chan JM, Tenet M, et al. Concurrent RB1 and TP53 Alterations Define a Subset of EGFR-Mutant Lung Cancers at risk for Histologic Transformation and Inferior Clinical Outcomes. J Thorac Oncol. 2019;14(10):1784-1793.
8. Niederst MJ, Sequist LV, Poirier JT, et al. RB loss in resistant EGFR mutant lung adenocarcinomas that transform to small-cell lung cancer. Nat Commun. 2015;11;6:6377.
9. Lee JK, Lee J, Kim S, et al. Clonal History and Genetic Predictors of Transformation Into Small-Cell Carcinomas From Lung Adenocarcinomas. J Clin Oncol. 2017;35(26):3065-3074.
10. Tokaca N, Wotherspoon A, Nicholson AG, et al. Lack of response to nivolumab in a patient with EGFR-mutant non-small cell lung cancer adenocarcinoma sub-type transformed to small cell lung cancer. Lung Cancer. 2017;111:65-68.