By Ricardo Sales dos Santos, MD, PhD, and Juliana Franceschini, PhD
Posted: June 24, 2020


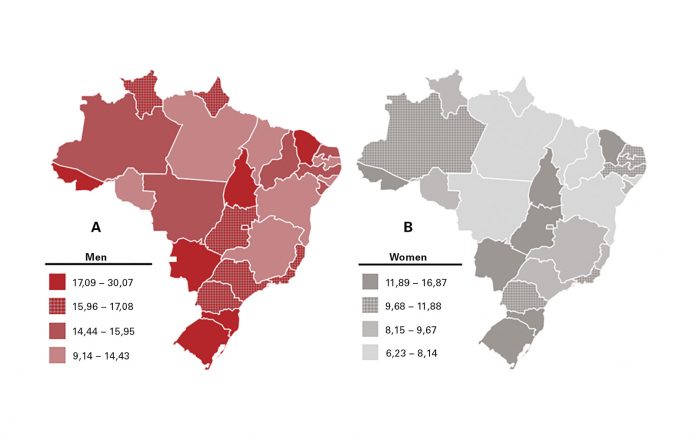
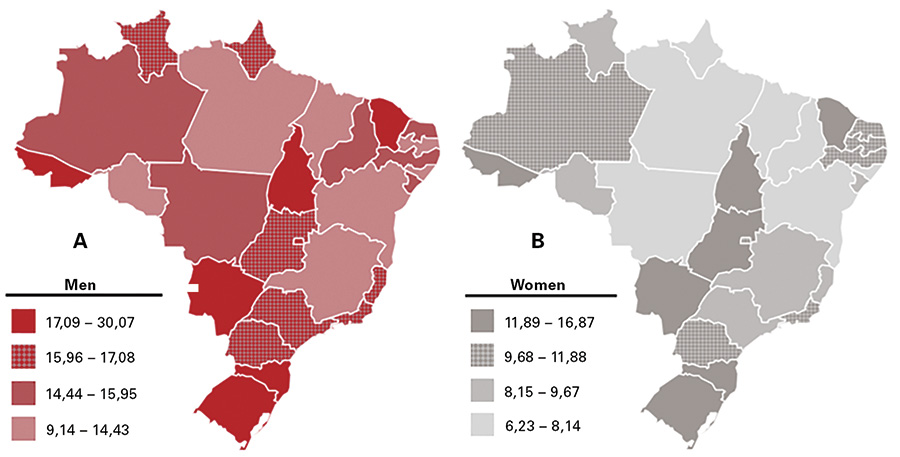
The reality of lung cancer in Brazil is as alarming as it is in the rest of the world. However, problems related to the diagnosis and treatment of lung cancer in Brazil are aggravated by intrinsic characteristics of the national health system. The lack of access to healthcare in certain regions interferes with the analysis of lung cancer incidence and mortality in the country. Each year, approximately 30,000 new cases of lung cancer are diagnosed in Brazil.1,2 The southern and southeastern regions have higher lung cancer prevalence rates (between 20 and 55 cases per 100,000 inhabitants) than the northern and northeastern states (less than 10 cases per 100,000 inhabitants; Fig.).3 A possible explanation for this fact lies in a broader coverage of cancer services in the South and Southeast regions of Brazil, which have more than twice as many specialized centers when compared to the other mentioned regions. The low supply of cancer services yields fewer diagnoses and possibly many deaths without a defined cause; this may be related to the diagnosis of lung cancer or other types of cancer.
Fortunately, there has been a major drop-off in smoking rates in Brazil since the 1980s, reducing the number of smokers by more than 50%, thanks to adherence to public policies on cigarette control with tax increases, a smoking ban in public places, and limitations on cigarette advertising.4-6
Diagnosis
Unfortunately, most cases of lung cancer in Brazil are diagnosed at an advanced stage; fewer than 10% of cases are diagnosed at an early stage (stages I and II).7 Symptomatic patients have great difficulty in securing a diagnosis in both the public and private healthcare systems. Various analyses of patients diagnosed with lung cancer show that most require multiple medical appointments and face difficulties in screening or work-up, delaying diagnosis by many weeks or months.4
According to a large cancer registry database study, which included a total of 35,018 patients diagnosed with NSCLC, and data from 258 hospitals in 25 states of Brazil and the Federal District (Brasília) between 2000 and 2011, a progressive increase occurred in the percentage of cases of advanced stages of NSCLC.8 Efforts have been made to promote expansion of cancer care to the Brazilian population in the Brazilian Public Health System (SUS). The Brazilian Ministry of Health implemented in 2000 the “Expande” Project, with the coordination of the National Cancer Institute of Brazil. The principal goals of this project were to expand access to cancer treatment in the country and also to reduce regional inequalities.9
Screening
Since the results of the National Lung Screening Trial were published in 2011,10 efforts have been made to implement screening programs in Brazil. Between 2013 and 2016, results of the first Brazilian national screening study (BRELT1) were published.11,12 BRELT1 validated low-dose CT imaging as a screening method in our region, which has a high rate of granulomatous disease. We noticed that this rate did not increase the number of biopsies nor did it affect the prevalence of lung cancer compared to other studies published in the northern hemisphere: biopsies were performed in approximately 3% of the 790 study participants, and diagnosis of early stage lung cancer occurred in 1.5% of participants. Despite these data, to date, there are no national public policies on the subject. Nor are there definitive statements from specialized national medical entities supporting screening as it should be supported.13 In this scenario, some medical institutions in different regions of the country have started isolated screening programs. At the moment the data from these programs are being consolidated for a more detailed discussion, in partnership with the “Propulmão” Program, an initiative of medical practitioners and healthcare professionals whose mission is to prevent lung cancer through education, awareness, and discussion on lung care.14
One of the basic and important barriers to lung cancer screening is the number of CT scanners in the public system, which is responsible for the healthcare of approximately 70% of the Brazilian population. The private system has six times more CT scanners, with numbers similar to those found in high-income countries.15
Overcoming Obstacles
Brazil has just over 700 thoracic surgeons and approximately 600 radiation oncologists, for an estimated population of more than 200 million. (In contrast to the United States, only general thoracic surgeons and not cardiothoracic surgeons are included in this specialty in Brazil.) Despite the reasonable number of professionals, there is a higher concentration of these individual in large centers, in cities with more than one million inhabitants (15 cities in the country, three of them in the state of São Paulo).16 Furthermore, there is a shortage of radiotherapy devices, with fewer than 250 units nationwide, and this greatly slows access to radiotherapy treatment.17
Since 2010, new technologies for the diagnosis and treatment of lung cancer have been established in different states, such as endobronchial ultrasound, robotic surgery systems, and ablative therapy equipment. However, it is noteworthy that the availability of appliances and especially disposable equipment is almost exclusive to the private healthcare system.18 By 2020, fewer than five public hospitals could be cited as one of the state-of-the-art lung cancer care providers nationwide.
Brazil is a country of continental dimensions which, despite having among the 10 largest economies in the world, still faces structural problems in sanitation, outbreaks of infectious diseases, and epidemics of communicable diseases. In addition, violence accounts for thousands of deaths each year.19 In this context, discussion about the treatment of lung cancer in advanced stages, with appropriate access to molecular tests and coverage of the costs of new drugs in precision oncology, confronts several practical and theoretical obstacles for wider availability to the population.20 In many cases, patients need to go to court to access high-cost medications in the public and private system. Access is further affected by the rapid advancement and specificities of the new technologies, which are often inaccessible either due to the clinical condition of the patients, many of whom are too ill to benefit, or due to competing priorities in the case of public health managers, who are compelled to cover high costs without the certainty of therapeutic efficacy.
However, headway is being made. There are promising initiatives involving research groups allied with the pharmaceutical industry to provide large-scale molecular testing for patients diagnosed with lung cancer. Some pharmaceutical companies offer molecular testing with free access to doctors and no charge for patients21-24; such partnerships should allow information on the occurrence of mutations and molecular biomarkers in our population to be reported, with better delineation of public policy in the acquisition of medicines.
In our opinion, one of the greatest challenges of the Brazilian health system is the need to integrate the activities of the private system with the public system, generating demand and access in an organized and structured way to various technologies already available in some regions. New value-based compensation models need to be quickly tested and made viable, at the risk of further disruption of the provision of medical services. ✦
About the Authors: Dr. Sales dos Santos is the head of Respiratory Medicine at Hospital Cárdio Pulmonar, Salvador/Bahia, Brazil. He works as staff thoracic surgeon at Hospital Israelita Albert Einstein, São Paulo, and CLION, Einstein’s Oncology Network, Salvador/Bahia, Brazil. He contributes as member of IASLC´s Screening & Early Detection Committee, ProAr Foundation, and Propulmão Program. Dr. Franceschini is a physical therapist and research coordinator at Propulmão Program, project manager at ProAr Foundation, and a postdoctoral researcher in the Respiratory Division, Universidade Federal de São Paulo/ UNIFESP, Brazil.
Visit JTO.org to read a more extensive article published in February 2020 about lung cancer prevention, diagnosis, and treatment in Brazil. Regional perspectives also are available for China, Italy, Canada, Saudi Arabia, and 14 other countries.
References:
1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424.
2. Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941-1953.
3. INCA. Estimativa 2018: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2017:128.
4. de Sa VK, Coelho JC, Capelozzi VL, de Azevedo SJ. Lung cancer in Brazil: epidemiology and treatment challenges. Lung Cancer (Auckl). 2016;7:141-148.
5. Monteiro CA, Cavalcante TM, Moura EC, Claro RM, Szwarcwald CL. Population-based evidence of a strong decline in the prevalence of smokers in Brazil (1989-2003). Bull World Health Organ. 2007;85(7):527-534.
6. Ministério da Saúde. Vigitel Brazil 2018: surveillance of risk and protective factors for chronic diseases by telephone survey: estimates of frequency and sociodemographic distribution of risk and protective factors for chronic diseases in the capitals of the 26 Brazilian states and the Federal District in 2018. Brasília: Ministério da Saúde; 2019:132.
7. Araujo LH, Baldotto C, Castro G, Jr., et al. Lung cancer in Brazil. J Bras Pneumol. 2018;44(1):55-64.
8. Costa G, Thuler LC, Ferreira CG. Epidemiological changes in the histological subtypes of 35,018 non-small-cell lung cancer cases in Brazil. Lung Cancer. 2016;97:66-72.
9. INCA. Expansão da Assistência Oncológica (Projeto EXPANDE) Rio de Janeiro: INCA. https://www.inca.gov.br/acesso-a-informacao/acoes-e-programas/projeto-expande. Published 2018 [updated July 17, 2018]. Accessed January 9, 2020.
10. Kramer BS, Berg CD, Aberle DR, Prorok PC. Lung cancer screening with low-dose helical CT: results from the National Lung Screening Trial (NLST). J Med Screen. 2011;18(3):109-11.
11. Santos RS, Franceschini JP, Chate RC, et al. Do Current Lung Cancer Screening Guidelines Apply for Populations with High Prevalence of Granulomatous Disease? Results from the First Brazilian Lung Cancer Screening Trial (BRELT1). Ann Thorac Surg. 2016;101(2):481-488.
12. Santos RS, Franceschini JP, Kay FU, et al. Lowdose ct screening for lung cancer in brazil: A study protocol | Rastreamento de cancer de pulmão por meio de TC de baixa dosagem no Brasil: Protocolo de pesquisa. J Bras Pneumol. 2014;40(2):196-199.
13. Mathias C, Prado GF, Mascarenhas E, et al. Lung Cancer in Brazil. J Thorac Oncol. 2020;15(2): 170-175.
14. Propulmão Program. http://www.propulmao.com.br/. Accessed January 9, 2020.
15. FIOCRUZ. A saúde no Brasil em 2030 – prospecção estratégica do sistema de saúde brasileiro: estrutura do fi nanciamento e do gasto setorial. 22 ed. Rio de Janeiro: Fiocruz/Ipea/ Ministério da Saúde/Secretaria de Assuntos Estratégicos da Presidência da República; 2013:168.
16. Tedde ML, Petrere Jr. O, Pinto Filho DR, et al. General thoracic surgery workforce: training, migration and practice profi le in Brazil. Eur J Cardiothorac Surg. 2015;47(1):e19-24.
17. Ministério da Saúde. Censo Radioterapia. Brasilia; 2019:10.
18. Interfarma. Câncer no Brasil – A jornada do paciente no sistema de saúde e seus impactos sociais e fi nanceiros. Associação da Indústria Farmacêutica de Pesquisa (Interfarma); 2019:88.
19. Reis C, Barbosa L, Pimentel VP. O desafio do envelhecimento populacional na perspectiva sistêmica da saúde. BNDES Setorial. 2016;44:37.
20. Kaliks RA, Matos TF, Silva VA, Barros LHC. Differences in systemic cancer treatment in Brazil: my Public Health System is different from your Public Health System. Braz J Oncol. 2017;13(44):12.
21. Bristol-Myers Squibb. IODetect. https://www.iodetect.com.br. Accessed January 9, 2020.
22. MSD. PD-Point – Programa de Biomarcador MSD. https://www.pdpoint.com.br. Accessed January 9, 2020.
23. Pfi zer. Pfi zerAlvo. http://alkalvo.com.br. Accessed January 9, 2020.
24. AstraZeneca. ID. http://www.programaid.com.br. Accessed January 9, 2020.
25. INCA. Neoplasia maligna da traqueia, dos brônquios e dos pulmões (taxas ajustadas). Rio de Janeiro: INCA. https://www.inca.gov.br/estimativa/taxas-ajustadas/neoplasia-malignada-traqueia-dos-bronquios-e-dos-pulmoes. Accessed May 20, 2020.










