This image was reproduced from a study by Lee J et al.1 with permission.
By Jin Mo Goo, MD, PhD, and Yeol Kim, MD, MPH, PhD
Posted: April 16, 2020


In 2015, based on the evidence from the National Lung Screening Trial, the Korean multisociety collaborative committee developed and published a guideline for lung cancer screening using low-dose CT (LDCT). The guideline recommends annual LDCT screening for three groups: high-risk smokers aged 55 to 74 years, with at least a 30 pack–year smoking history; current smokers; and former smokers who quit smoking within 15 years.
Based on this guideline and previous studies of lung cancer screening with LDCT, the Korean Lung Cancer Screening Project (K-LUCAS) was launched to evaluate the feasibility of implementing a population-based lung cancer screening program in South Korea.1 This was a 2-year project to enroll 8,000 participants at 14 institutions. For the nodule management and reporting, the Lung CT Screening Reporting and Data System (Lung-RADS) from the American College of Radiology was adopted.2 Requirements for CT scanners and acquisition parameters include multidetector CT with a minimum of 16 channels, complete scan with one-breath hold, section thickness of 1.25 mm or less, and a volume CT dose index of less than 3.0 mGy for average-sized patients (170 cm/70 kg; body mass index, 24 kg/m2). A total of 13,692 individuals underwent LDCT for the K-LUCAS, and lung cancer was detected in 79 patients as of April 2019. Among them 68.4% of cancers were stage I or II, which is much higher than that of the general population (29.6%), showing a potential for stage shift of lung cancer with lung cancer screening. Based on these results, a national population-based lung cancer screening program began in July 2019 in South Korea.
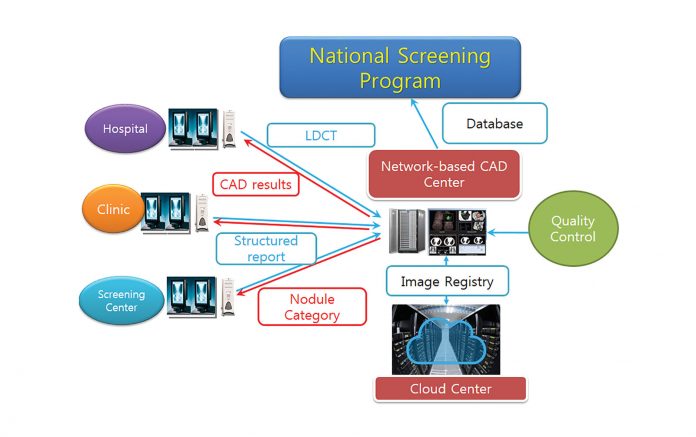
Necessity for the Cloud-Based Computerized System
To achieve lung cancer mortality reduction with more benefit than harm, a high-quality lung cancer screening program with LDCT is required. A cloud-based computerized system may provide many advantages for this purpose.
In the Lung-RADS, the category of a nodule is determined by the nodule consistency (whether it is a solid nodule, partsolid nodule, or ground-glass nodule), and the size of the nodule is determined by averaging its bidimensional measurements. By employing an automated nodule- segmentation program, reader agreement can be improved. Once a nodule is segmented, it can be easily converted to either diameter or volume values. A computer-aided detection (CAD) system can enhance the detection performance of readers. With the computerized support, the results can be effectively reported without an erroneous categorization of Lung-RADS.3
In quantitative imaging, there are many sources of variability, and the software itself is one cause of variability. If we use different software, it will generate different nodule volume, which will subsequently affect the backbone of nodule management: the size and volume doubling time of a nodule. A thin-client approach using a cloud system is a promising approach to help deal with this issue. By checking the imaging protocol stored in Digital Imaging and Communications in Medicine (DICOM) of CT data, which are uploaded in the cloud system, quality control of CT data, such as section thickness and radiation dose, can be easily applied. In Korea, many patients visit different hospitals due to a variety of reasons, and they usually need to carry a CD (or DVD) with medical images. Because comparison with previous CT scans is essential in lung cancer screening, a cloud system is an effective tool to enhance workflow and reduce cost and inconvenience. Data collected in the system will provide answers to research questions and help to establish future policies in lung cancer screening.
Establishment of the System
Initially, the K-LUCAS started with a conventional reading system (visual assessment and manual measurement at PACS). The cloud-based computerized system was fully established in November 2018 (Fig.). Because it was the first medical usage of a cloud system in a public sector, it took a long time to receive approval from multiple departments of the government. CT data were uploaded to a cloud center through a virtual private network from 14 participating hospitals. As soon as the data were uploaded, a CAD program (Visia, MeVis) automatically generated CAD results. Radiologists used a viewer program (AVIEW, Coreline Soft) with a thin-client approach, which provided nodule segmentation, categorization, and reports. Readers could see the CAD results after initial review of CT images and were allowed to modify the segmentation results if they were not satisfactory. Final decisions were made by radiologists at each hospital, and these results were stored in the cloud system. In the second year, if section thickness or radiation dose of CT scans did not meet the protocol guidelines, the system posted a red flag in the worklist of the program.
Preliminary Results
When a survey was conducted among participating radiologists, most favored the cloud-based system over a conventional reading system. After installing the computerized system, an increase in positive rates of lung cancer screening was noticed. The increased positive rate was mainly caused by a larger average diameter on a three-dimensional plane in a computerized system than an average diameter on transverse planes in manual measurements. Therefore, the measurement plane was modified to orthogonal planes in a computerized system according to the Fleischner Society recommendations.
In the K-LUCAS, a conventional reading was performed initially, which was replaced by a computerized system. When the two systems were compared, the computerized system resulted in detection of more nodules while reducing variability in positive Lung-RADS rates among institutions. Further analyses are being conducted to compare the institutional reading with the retrospective central review.
Challenges and Future Directions
Protecting personal information is a big hurdle in implementing a cloud-based system in Korea. Therefore, although this system is now partially integrated into the Korean National Cancer Screening Program after the K-LUCAS, all data are anonymized, and the access to the cloud is limited to the corresponding hospital where the participant underwent LDCT. Therefore, further analysis or use of these data for follow up is not possible at the moment. Hopefully this issue will be resolved when this system is installed in the National Health Insurance Service in a few years.
With recent advances in artificial intelligence techniques, we expect that the performance of nodule detection and segmentation programs to improve. In addition, smoking-related diseases such as chronic obstructive pulmonary disease and coronary artery disease can also be assessed by emphysema quantification and analysis of coronary artery calcification. By combining data extracted from LDCT, predicting the risk and prognosis of lung cancer will be feasible. ✦
About the Authors: Dr. Goo is a professor in the Department of Radiology, Seoul National University Hospital; president of the Korean Society of Imaging Informatics in Medicine; and director of the Institute of Radiation Medicine, Seoul National University Medical Research Center. Dr. Kim is a board-certified family physician at the Center for Cancer Prevention and Detection and the Smoking Cessation Clinic, Hospital, NCC. Dr. Kim is the principal investigator of K-LUCAS.
References:
1. Lee J, Lim J, Kim Y, et al. Development of Protocol for Korean Lung Cancer Screening Project (K-LUCAS) to Evaluate Effectiveness and Feasibility to Implement National Cancer Screening Program. Cancer Res Treat. 2019;51(4):1285-1294.
2. Lee JW, Kim HY, Goo JM, et al. Radiological Report of Pilot Study for the Korean Lung Cancer Screening (K-LUCAS) Project: Feasibility of Implementing Lung Imaging Reporting and Data System. Korean J Radiol. 2018;19(4):803-808.
3. Han DH, Goo JM, Chong S, Ahn MI. Are Lung Imaging Reporting and Data System Categories Clear to Radiologists? A Survey of the Korean Society of Thoracic Radiology Members on Ten Difficult-to-Classify Scenarios. Korean J Radiol. 2017;18(2):402-407.
Related article: Korean Lung Cancer Screening Project (K-LUCAS) Led to Launch of New National Lung Cancer Screening Program in Korea