By Julien Mazières, MD, PhD, and Julie Milia, PhD
Once considered a “man’s disease,” lung cancer no longer discriminates. During the last decade, lung cancer in women has become the most common cause of cancer death in women in the US, surpassing breast cancer, and the second leading cause of cancer death in women in Europe. Lung cancer in women displays specific epidemiological, radiological, clinical, and pathological characteristics that differentiate it from lung cancer in men. Moreover, both prognosis and response to treatment appear to be different from men. In line with these findings, lung carcinogenesis is, at least in part, distinct in women and involves different mechanisms and signaling pathways. We therefore believe that specific therapeutic strategies should be considered in women harboring lung cancer.
Epidemiology
Lung cancer is the most common cancer in men worldwide (1.2 million), with the highest rates in central and eastern Europe (53.5 per 100,000) and eastern Asia (50.4 per 100,000). In women, the incidence rates are generally lower. The highest estimated rates are in northern America (33.8), northern Europe (23.7), and eastern Asia (19.2), compared to much lower rates in western and middle Africa (1.1 and 0.8, respectively).1 Denmark has the highest rate of lung cancer in women, followed by Canada and US. In the US, the rate of new lung cancer cases over the past 37 years has dropped for men (28% decrease), while it has risen for women (98% increase).
The number of lung cancer deaths worldwide will increase from 1.6 million in 2012 to 3 million in 2035. Consequently, the number of lung cancer deaths will almost double in both men (1.1 million in 2012 to 2.1 million in 2035) and in women (0.5 million in 2012 to 0.9 million in 2035).2
Presentation
Lung cancer in females exhibits some specificity such as a higher frequency of adenocarcinoma (64% for women vs 48% for men) and a higher incidence of tumors with a lepidic component.3 There is a higher proportion of non-smokers among women with lung cancer than in men: 30% vs 10%, respectively. This rate can rise as high as 80% in Asia.4 Finally, females have a generally better prognosis and their tumors are more chemosensitive in comparison to males.5
Potential Risk Factors
Tobacco
Smoking accounts for about 90% of global lung cancer deaths in men and 70% of the deaths in women.6 Tobacco remains the major risk factor for women today. Women appear to be more sensitive to carcinogens; for the same quantity of tobacco consumption, they will develop more cancer than men.5 This may be explained in part by lower expression of DNA repair genes such as ERCC, BRCA1, and RRM1 in women as compared to men.7
Environment
In Asia, lung cancer in women has been correlated to the Kang use (charcoal oven); and in Denmark, more lung cancers have been detected in women bus and tramway drivers.8 In other countries, no real links have been made between a specific “women’s environment” and lung cancer incidence.
Hormones:
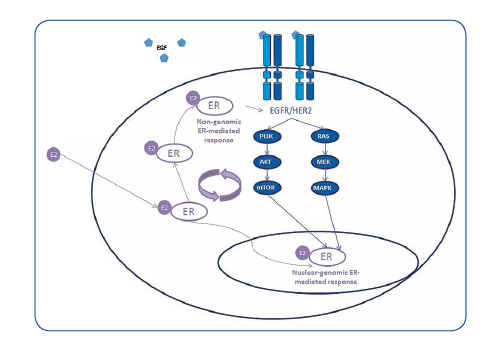
Women diagnosed with lung cancer have better clinical outcomes compared to men within the same strata of stage and histology. Several studies support a link between female hormones and lung cancer: early menopause, less than three pregnancies, a short menstrual cycle, use of estrogenic substitutes, and a family history of hormone-dependent cancers.3,9,10,11 Estrogens may be involved in lung cancer carcinogenesis, and estrogen receptors (ERs), mainly ERbeta, are present and functional in normal lung and tumor cell lines and tissues. Estrogen can directly stimulate the transcription of estrogen-responsive genes in the nucleus of lung cells, and it can also transactivate growth factor signaling pathways, in particular the epidermal growth factor pathway12 (Figure 1). Moreover, treatment with hormonal substitutes negatively affects the prognosis of women with stage IV lung cancer.13
Genetics
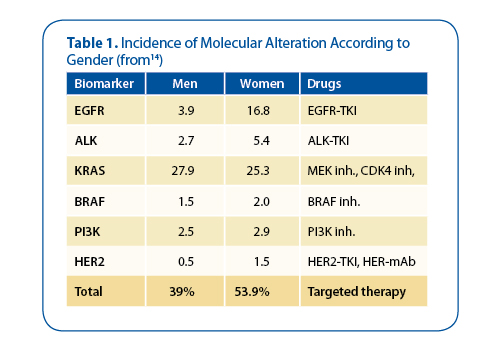
Routine molecular profiling of patients with advanced NSCLC has been conducted in France, and the results underscore differences based on gender: 54% of women carry known genetic alterations, whereas these are present in only 39% of men, except for KRAS, which is more frequent for men14 (Table 1).
The incidence and mortality of lung cancer are still increasing in Asian females, who are mostly never-smokers, and presents as adenocarcinoma. Druggable oncogenic drivers are more prevalent in Asian females, so their disease has a higher opportunity to use targeted therapy. The identification of specific genetic alterations or normal profiles may serve as new therapeutic targets.—Caicun Zhou, PhD, MD Shanghai Pulmonary Hospital, Shanghai, China, IASLC Lung Cancer News Associate Editor
Therapeutic Strategies
To date, there are no recommendations to treat men and women differently. Nevertheless, the incidence of molecular alteration is higher in women and led tomore frequent use of targeted therapies (Table 1). EGFR-activating mutation is found in around 20% of the women, with the incidence as high as 40% in non-smokers. Tyrosine kinase Inhibitors (TKIs) are now the standard treatment for the care of EGFR-mutated patients.15 ALK rearrangements are also found more often in women than in men: 5.4% vs 2.7%, according to the biomarkers study performed in France.14 The HER2 mutation is also more frequently found in women. The use of antibodies targeting HER2 for these patients seems to yield promising overall response rates.16
Hormones are also known to play an important role in oncogenesis and development of NSCLC because estrogen can stimulate cell proliferation and antiestrogens can cause inhibition of proliferation. We have increasing data on the interactions between estrogen receptors and EGFR signaling pathways, as well as on the additive antitumor effect of antiestrogens (tamoxifen and fulvestrant) combined with tyrosine kinase inhibitors (gefitinib, erlotinib, and vandetanib).12,17 Thus, future treatment may add antihormonal drugs to targeted therapies. Some trials such as LADIE-IFCT1003 trial (NCT01556191) are currently testing this hypothesis.
In summary, we think that lung cancer in women, at least in part, is a distinct entity with distinct carcinogenesis. We propose that improving knowledge of its biology will permit the identification of specific genetic alterations or hormonal profiles that may serve as new therapeutic targets. ✦
References
1. Ferlay J, Soerjomataram I, Dikshit R, et al: Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. International Journal of Cancer 136:E359- 86, 2015.
2. Didkowska J, Wojciechowska U, Manczuk M, et al: Lung cancer epidemiology: contemporary and future challenges worldwide. Ann Transl Med 4:150, 2016.
3. Zatloukal P, Kubik A, Pauk N, et al: Adenocarcinoma of the lung among women: risk associated with smoking, prior lung disease, diet and menstrual and pregnancy history. Lung Cancer 41:283-93, 2003.
4. Shafer D, Albain K: Lung cancer outcomes in women. Semin Oncol 36:532-41, 2009
5. Radzikowska E, Glaz P, Roszkowski K: Lung cancer in women: age, smoking, histology, performance status, stage, initial treatment and survival. Population-based study of 20 561 cases. Ann Oncol 13:1087-93, 2002.
6. Ezzati M, Lopez AD: Estimates of global mortality attributable to smoking in 2000. Lancet 362:847- 52, 2003.
7. Planchard D, Loriot Y, Goubar A, et al: Differential expression of biomarkers in men and women. Semin Oncol 36:553-65, 2009.
8. Soll-Johanning H, Bach E, Olsen JH, et al: Cancer incidence in urban bus drivers and tramway employees: a retrospective cohort study. Occup Environ Med 55:594-8, 1998.
9. Seow A, Poh WT, Teh M, et al: Diet, reproductive factors and lung cancer risk among Chinese women in Singapore: evidence for a protective effect of soy in nonsmokers. Int J Cancer 97:365- 71, 2002.
10. Gao YT, Blot WJ, Zheng W, et al: Lung cancer among Chinese women. Int J Cancer 40:604-9, 1987.
11. Taioli E, Wynder EL: Re: Endocrine factors and adenocarcinoma of the lung in women. J Natl Cancer Inst 86:869-70, 1994.
12. Stabile LP, Lyker JS, Gubish CT, et al: Combined targeting of the estrogen receptor and the epidermal growth factor receptor in non-small cell lung cancer shows enhanced antiproliferative effects. Cancer Res 65:1459-70, 2005.
13. Ganti AK, Sahmoun AE, Panwalkar AW, et al: Hormone replacement therapy is associated with decreased survival in women with lung cancer. J Clin Oncol 24:59-63, 2006.
14. Barlesi F, Mazieres J, Merlio JP, et al: Routine molecular profiling of patients with advanced non-small-cell lung cancer: results of a 1-year nationwide programme of the French Cooperative Thoracic Intergroup (IFCT). Lancet, 2016.
15. Rosell R, Carcereny E, Gervais R, et al: Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 13:239-46, 2012.
16. Mazieres J, Barlesi F, Filleron T, et al: Lung cancer patients with HER2 mutations treated with chemotherapy and HER2-targeted drugs: results from the European EUHER2 cohort. Annals of Oncology, 2015.
17. Siegfried JM, Gubish CT, Rothstein ME, et al: Combining the multitargeted tyrosine kinase inhibitor vandetanib with the antiestrogen fulvestrant enhances its antitumor effect in non-small cell











