By Erik J. MacLaren, PhD
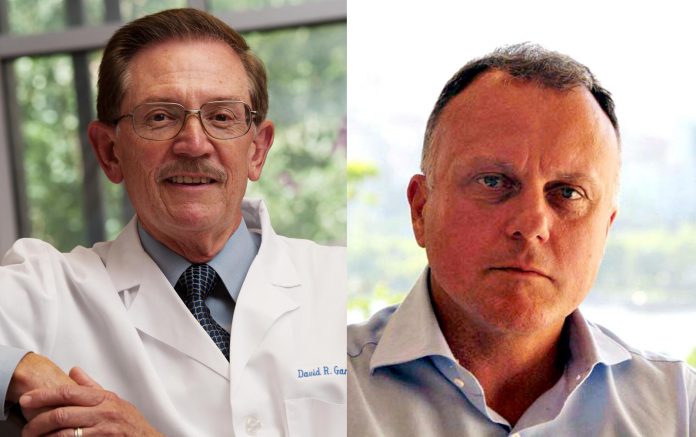
Osimertinib, a third-generation epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI), received FDA approval in November 2015 for use in patients with metastatic EGFR T790M non-small cell lung cancer (NSCLC) whose disease has progressed on other EGFR TKIs. Data presented in April 2016 at the European Lung Cancer Conference suggest that this drug may also be effective as a first-line treatment for EGFRmutated NSCLC. IASLC Lung Cancer News discussed the impact of these developments with David R. Gandara, MD, Director of the Thoracic Oncology Program at the University of California Davis Comprehensive Cancer Center in Sacramento, California, and immediate Past Chair of the Southwest Oncology Group Thoracic Committee, and with Federico Cappuzzo, MD, PhD, Director of Medical Oncology, AUSL Romagna, in Ravenna, Italy.
Q: What kind of impact has osimertinib had on the management of NSCLC with the EGFR T790M mutation?
Gandara: Osimertinib, a third-generation EGFR TKI, has rapidly become standard of care (SOC) for patients after disease progression (PD) on a first- or second-generation TKI, in patients with cancers harboring the T790M resistance mutation. In this setting, it produces a very good response rate, about 60%, and an excellent progression-free survival (PFS) outcome. Furthermore, it is associated with an acceptable toxicity profile, as it has low affinity for wild-type EGFR.
Cappuzzo: Osimertinib is an attractive agent because it is very potent; it has been designed particularly to overcome resistance to first- or second-generation EGFR TKIs, including erlotinib, gefitinib, or afatinib. Osimertinib is also active against brain metastases and leptomeningeal disease. These properties render this agent very attractive and very promising in patients with NSCLC.
Q: What are the prospects that osimertinib will displace standard first-line TKIs, and what level of evidence would secure its role in the first-line?
Gandara: We will have to await the results of the ongoing FLAURA trial,1 which compares osimertinib with investigator choice of either gefitinib or erlotinib, to answer these questions. Some critics will say that FLAURA did not go up against afatinib, the second-generation TKI that has shown some evidence of superiority over gefitinib in the LUX LUNG 7 trial, so the impact of FLAURA, if it is positive, will be in the eyes of the beholder.
In terms of level of evidence, FLAURA is a large trial, with about 650 patients planned, and PFS as the primary endpoint. If it meets that endpoint in a clinically meaningful way, which would be an improvement by several months for osimertinib compared to control or a hazard ratio of 0.7 or lower, it will be sufficient to change practice. However, I should note that none of the trials comparing erlotinib or gefitinib to chemotherapy have ever demonstrated improvement in overall survival. If FLAURA were to show improvement in overall survival, that could certainly propel it forward in terms of therapy.
Cappuzzo: The activity of these agents has been investigated in TKI-naive patients,2 and the response rate, duration of response, and PFS in this population were quite impressive. To move to a firstline setting, certainly we need phase III trial data, which will clarify whether we can use osimertinib in the firstline. Preliminary data strongly suggest that this agent could become the new SOC in the front-line setting, but I repeat: we need a phase III trial to confirm such findings.
Q: If osimertinib does move to the first-line, where does that leave us in the second-line setting? Does chemotherapy become the “default” option?
Gandara: This issue, about what to do in second-line if osimertinib moves into first-line, is perhaps the most confounded right now. In my mind, there is no clear-cut answer, since checkpoint immunotherapy agents, although approved in the second-line setting, seem to produce relatively poor results in patients with EGFR-mutated lung cancers, likely due to the low mutational load in these oncogene-driven cancers. That would mean that platinum-based chemotherapy would become the secondline choice, unless a new TKI with activity against osimertinib resistance—for example, the C797S mutation—emerges in the near future.
Cappuzzo: We know that the main mechanism related to osimertinib failure is the occurrence of a new secondary mutation, C797S, but we do not yet have clinical data. Based on preclinical models, it seems that if the C797S mutation is present but T790M is not, the patient may still be sensitive to firstgeneration EGFR TKIs. Assuming that osimertinib becomes the standard frontline therapy, it will be crucial to understand whether the patient is still sensitive to other currently available agents. That will require prospective clinical data on this issue. I think chemotherapy remains an important option for patients with EGFR mutations, but only after failure on all available EGFR TKIs.
Q: Will we automatically be obtaining repeat biopsies or liquid biopsies in the setting of acquired resistance?
Gandara: This question has already been answered, in my opinion, with guidelines from 2013 onward, such as those from IASLC, along with clinical practice patterns already showing that a repeat biopsy at time of resistance is critical in the decision-making process. Importantly, testing needs to extend beyond T790M, to look for other mechanisms of resistance in addition to T790M. We know that this occurs in about half of cases.
We are now in a transition phase between repeat tissue biopsy and socalled liquid biopsy for plasma cell-free DNA analysis. In some patients, repeat biopsy is simply not possible. Further, the ability to perform liquid biopsy through an NGS platform is revolutionary, and I believe it will become the SOC very Osimertinib from page 1 Gregory A. Curt, MD soon. The sensitivity is very high now, and there are essentially no false positives. In fact, recent data suggest that if testing for T790M, for example, is negative in tissue repeat biopsy but positive in plasma, that it is the tissue that is a false negative, not the reverse. That being said, a very small number of patients will have evolution to small cell lung cancer after a first-line EGFR TKI, and that can only be detected by biopsy at present.
Cappuzzo: We know that the biology of the tumor changes during treatment because of the occurrence of different secondary mutations, and that it is extremely important to identify the mechanism of resistance to determine the best subsequent therapy. It is, therefore, extremely important to repeat the biopsy of the tumor; however, we know that in clinical practice this is not always done. Liquid biopsy is a very attractive alternative, and many centers are already doing these tests. I strongly believe that this technology will become the SOC for our patients.
Q: What role, if any, do you think urine assays will play in NSCLC?
Gandara: Urine testing has recently been shown to be complementary to tissue and plasma, but right now has a more limited scope in terms of number of genes assessed. We will have to wait and see how this evolves, because eventually insurance companies or governmental agencies are going to want to pay for only one test: tissue biopsy or plasma cfDNA or urine, not two or three tests.
Cappuzzo: We can obtain information from the blood, but we can also try to obtain some information from the urine. It is possible that we could ultimately combine different tests because we know that there is not 100% overlap in the results of these different assays; by so doing, we could significantly reduce the risk of false-negative results. This is a very important consideration in clinical practice, ensuring that all patients have the opportunity to receive the right drug.
References
1. ClinicalTrials.gov. AZD9291 Versus Gefitinib or Erlotinib in Patients With Locally Advanced or Metastatic Non-small Cell Lung Cancer (FLAURA). 2014; https://clinicaltrials.gov/ct2/show/NCT02296125. Accessed June 26, 2016.
2. S. Ramalingam, J. C. Yang, C. K. Lee, et al. LBA1_PR – Osimertinib as first-line treatment for EGFR mutation-positive advanced NSCLC: updated efficacy and safety results from two Phase I expansion cohorts. Journal of Thoracic Oncology. 2016;11(4, Supplement):S152.