By James L. Mulshine, MD, PhD, Fred Hirsch, MD, PhD, and John K. Field, PhD, FRCPath
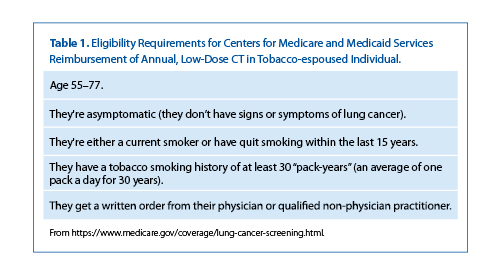
Over the last fifteen years, the use of lowdose computed tomography (LDCT) for early lung cancer detection in high-risk individuals has moved from the seminal study arising from an NIH-funded R01 grant,1 to the publication of the validation results of the National Lung Screening Trial (NLST),2 to the endorsement of the United States Preventive Services Task Force.3 Now in mid-March 2016, the Center for Medicare and Medicaid (CMS) has announced the details of its reimbursement approach (Table 1) for annual LDCT for lung cancer screening (https://www.medicare.gov/coverage/lung-cancer-screening.html).
Given the previous pace of progress with early lung cancer screening, this represents a swift transition, but the foundation of research supporting this transition has been considerable in volume and international in scope. For example, the rate of Stage I detection reported by the I-ELCAP at 81% seemed remarkably high compared to the expected 15%, but subsequent reports from the NLST (63%), the Dutch/Belgian NELSON (73.7%) and now the UK pilot study (66.7%), have consistently confirmed that routine early stage detection of lung cancer can be realized.1,2,4,5 Concerns have been reported about challenges with high rates of unproductive diagnostic workup rates from 28% with NLST, but more recent reports of 12% with the NELSON study suggest more efficient approaches are possible. The new American College of Radiology LungRADs approach leverages the College’s vast experience with breast cancer screening; when these criteria were applied retrospectively to the NLST cases, they were also able to achieve a low (12%) false-positive workup rate.6,7 Another recent report by I-ELCAP involved the re-analysis of archival data from the outcomes of over 20,000 subjects who had undergone screening and for which clinical outcome was known. In their retrospective analysis, the data suggested that nodules smaller than 7 mm could be followed with an LDCT one year later without sacrificing curability of screen-detected lung cancers.8
Fortunately, screening subjects demonstrate the ability to deal adaptively with the complex information inherent to the screening process. For participants in the NLST receiving a false-positive or a significant incidental finding with their screen result, they reported no significant difference in their health-related quality of life or anxiety outcomes at 1 or at 6 months after screening compared to individuals with negative screening results.9
Additional efforts to ensure quality in implementing lung cancer screening services are being conducted by the lung cancer patient advocacy group, Lung Cancer Alliance (LCA), which established in 2012, the National Framework for Screening Excellence in the Continuum of Care. This is a consortia of medical centers adhering to responsible best practices for safe and effective lung cancer screening. Currently, 400 institutions have joined this national network and been designated by LCA as Screening Centers of Excellence. This consortium is demonstrating how lung cancer screening can be scalable and replicable in different care settings by following best-practice criteria. LCA convenes annual screening conferences and maintains regularized contact with the national network to ensure there is a forum to exchange timely information on policy, research, best practices, and lessons learned. This forum and furthering the national dialogue on the screening process is critical to ensure optimal dissemination of this new preventive service.10
Fortunately, research to further improve the screening process continues to emerge at a rapid pace. For example, 2 reports recently evaluated the use of computer-assisted diagnostic (CAD) software systems to analyze the CT data for the presence of potential lung cancers. Yankelevitz and co-workers used computer- assisted visualization of potential lung cancers in a test set of 50 lung cancers, which was then analyzed by 4 different CAD tools. For baseline cancer detection, the systems varied between 56% and 70% accuracy in detecting the nodules, which were on average 4.8 mm.11 When comparable analysis was performed on scans acquired a year later, the systems ranged between 74% and 82% accuracy in detecting lung cancer in nodules that were on average 11.4 mm. Overall, the CAD systems detected 70% of lung cancers that were not initially detected by the radiologist, but failed to detect about 20% of the lung cancers when they were identified by the radiologist.11 An earlier study from the Dutch/Belgian group also found that CAD performed well. An analysis of 400 low-dose chest CT examinations from the NELSON trial documented 78.1% sensitivity of nodule detection for double reading by radiologist and 96.7% for CAD tool analysis.12 The conclusion based on these 2 studies is that CAD is likely to emerge as an important tool in improving the accuracy of radiological detection of lung cancer in the screening setting, but additional research is needed to fully validate how integrating CAD into the screening process can be most beneficial.
Lung cancer screening is a complex process that involves a number of steps all of which could contribute to the success or failure of the screening process.13 This brief report only touches on a few examples. Clearly, comprehensive, ongoing analysis to ensure the quality, accessibility and consistency of the delivery of this service is essential. In addition to the National Framework, the American College of Radiology, the Quantitative Imaging Biomarker Alliance, and CMS are establishing approaches to address the various components of the screening process.6,14 As Canada and China are now considering nationwide implementation of screening, growing experience with this new service should enable continued optimization of the screening process.15,16 ✦
References
1. Henschke CI, McCauley DI, Yankelevitz DF, et al. Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet. 1999–Elsevier.
2. Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011; 365:395-409.
3. Humphrey LL, Deffebach M, Pappas M, et al. Screening for lung cancer with low dose computed tomography: a systematic review to update the U.S. Preventive Services Task Force recommendation. Ann Intern Med. 2013; 159:411-420.
4. van Klaveren RJI, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med. 2009; 361:2221-2229.
5. Field JK, Duffy SW, Baldwin DR, et al. UK Lung Cancer RCT Pilot Screening Trial: baseline findings from the screening arm provide evidence for the potential implementation of lung cancer screening. Thorax. 2016; 71:161-170.
6. Kazerooni EA, Armstrong MR, Amorosa JK, et al. ACR CT accreditation program and the lung cancer screening program designation. J Am Coll Radiol. 2015; 12:38-42.
7. Pinsky PF, Gierada DS, Black W, et al. Performance of Lung-RADS in the National Lung Screening Trial: a retrospective assessment. Ann Intern Med. 2015; 162:485-491.
8. Henschke CI, Yip R, Yankelevitz DF, et al. Definition of a positive test result in computed tomography screening for lung cancer: a cohort study. Ann Intern Med. 2013; 158:246-252.
9. Gareen IF, Duan F, Greco E, et al. Impact of lung cancer screening results on participant health-related quality of life and state of anxiety in the National Lung Screening Trial. Cancer. 2014;120:3401-3409.
10. Mulshine JL, Sullivan D. Lung Cancer Screening, Invited Review. N Engl J Med. 2005; 352:42-48.
11. Liang M, Tang W, Xu DM, et al. Low-dose CT screening for lung cancer: Computer-aided detection of missed lung cancers. Radiology. 2016;150063. PMID: 27019363.
12. Zhao YI, de Bock GH, Vliegenthart R, et al. Performance of computer-aided detection of pulmonary nodules in low-dose CT: comparison with double reading by nodule volume. Eur Radiol. 2012;22:2076-2084.
13. Mulshine JL, D’Amico A. Issues with implementing a high-quality lung cancer screening program. CA Cancer J Clin. 2014;64:352-363.
14. Kazerooni EA, Armstrong MR, Amorosa JK, et al. ACR CT accreditation program and the lung cancer screening program designation. J Am Coll Radiol. 2015;12:38-42.
15. Mulshine JL, Gierada DS, Amato SG, et al. Role of the quantitative imaging biomarker alliance in optimizing CT for the evaluation of lung cancer screen-detected nodules. J Am College Radiol. 2015;12:390-395.
16. Zhou QH, Fan YG, Bu H, et al. China national lung cancer screening guideline with low-dose computed tomography (2015 version). Thorac Cancer. 2015;6:812-818.
17. Canadian Task Force on Preventive Health Care. Recommendations on screening for lung cancer. CMAJ. 2016. Published online