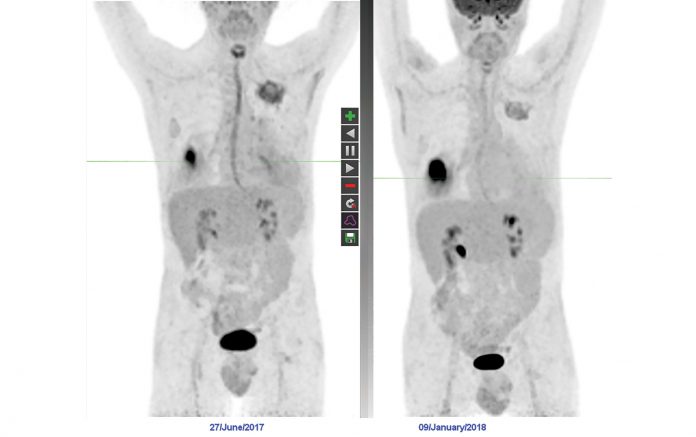
A breathless 59-year-old male cannabis smoker was found to have multiple FDG-avid pulmonary nodules (Left Panel). Biopsy of the left upper lobe nodule showed changes consistent with aspergillus infection. After antifungal therapy, repeat PET/CT imaging showed reduction in size and FDG avidity in all nodules except the right lower lobe nodule, which enlarged (Right Panel). Biopsy of this lesion showed squamous carcinoma. This T2N0M0 tumor subsequently responded to SABR.
By Michael MacManus, MD, FRANZCR, and Tim Akhurst, MD, FRACP
Posted: March 1, 2019

18F-FDG PET/CT scans portray living biology and are indispensable in thoracic oncologic evaluations, including presurgical staging of NSCLC, patient selection and target-volume definition in curativeintent radiation therapy (RT), and the evaluation of patients with suspected recurrence after definitive therapy. FDG-PET is also superior to CT for response assessment after definitive chemoradiation.1 The indications for PET/CT will continually expand as thoracic oncology becomes more complex with new immunotherapies and tyrosine kinase inhibitors (TKIs) and with the increasing use of stereotactic ablative body radiotherapy (SABR).2 Physicians interpreting PET must be aware of the clinical state of the patient beyond a simple request for “lung cancer imaging,” and they must fully understand the nuances regarding acquisition and interpretation of PET/CT scans.
The Importance of Standardization, Timing
PET data, including semi-quantitative variables such as tumor standardized uptake value, are profoundly influenced by technical factors, including patient preparation (e.g., avoidance of strenuous exercise, adequate fasting, hydration, and hyperglycemia) and appropriate FDG dosing. Standardization of image-acquisition timing after FDG injection and use of the same scanner and reconstruction protocols for all patient examinations contribute to accurate reading of serial scans.

Lung cancer can progress rapidly, especially in locoregionally advanced cases. PET/CT scans must be current at the time of commencement of curativeintent treatment; outdated or incorrectly acquired scans should be repeated. One study showed that more than 30% of patients with NSCLC eligible for chemoradiation had disease that progressed significantly within a median of 3 weeks between PET/CT scans, mandating changes to therapy.3 Baseline PET scans may provide additional clinical information, including identification of recurrent laryngeal nerve palsies, cardiac disease, unsuspected second malignancies, as well as otherwise “occult” CT-undetectable metastases. Differential FDG-PET response of apparently infective lesions to antimicrobial therapy might unmask unsuspected cancer (Fig. 1).
RT Planning, Assessing Therapeutic Response
Incorporation of FDG-PET data into RT planning frequently changes RT target volumes, often allowing better management of small FDG-avid nodes or preventing unnecessary irradiation of atelectatic lung. PET/CT scans acquired in the raised-arm RT position can be used directly for tumor-volume contouring and definition of planning target volumes.4 If a staging PET/CT scan can also be used for RT target definition, the PET request should make this clear, enabling proper patient positioning and facilitating cost savings and patient convenience.
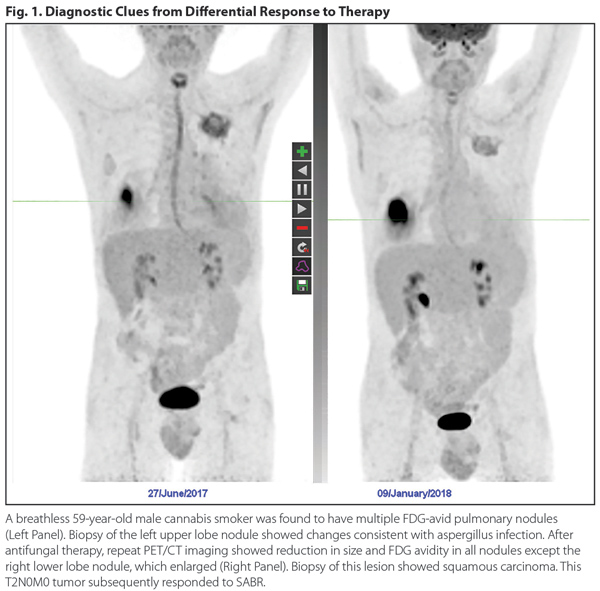
After curative-intent chemoradiation, the qualitative distinction between complete metabolic response (CMR; which is associated with a 5-year survival of approximately 50% of patients) and non-CMR (wherein prognosis is dramatically worse), can help determine further disease management, including salvage surgery or immunotherapy. Knowledge of typical uptake patterns in lung and pleura after RT is essential to avoid misinterpreting radiation-induced changes as persistent or progressive disease. After SABR for lung cancer, a nonmalignant pseudotumor may develop at the irradiated site; FDG-PET negativity can distinguish between a pseudotumor and local progression (Fig. 2). In the assessment of response to systemic therapy, the degree of partial metabolic response as assessed by semiquantitative analysis, such as PERCIST,5 which includes PET parameters unlike RECIST, can help determine whether to continue treatment.
Patterns of failure vary from progression at multiple sites to oligoprogression at a single or a limited number of sites. Delivery of locally ablative therapy to sites of oligoprogression identified by PET can allow continuation of otherwise efficacious therapy. FDG-PET has an important role in selection of patients suitable for metastasectomy or ablative techniques including SABR and radiofrequency ablation.
Newer Systemic Therapies
Therapy for lung cancer is evolving rapidly, with the advent of multiple novel systemically administered agents, each characterized by specific therapeutic and toxic effects that may influence PET/ CT evaluation. Molecularly targeted therapies, especially TKIs targeted to activating mutations involving EGFR, EML4-ALK, BRAF, and ROS1, have revolutionized the care of many patients with lung cancer who harbor the specific targets for these agents. Immunotherapy, particularly the immune checkpoint inhibitors, have generated well-founded excitement due to improvements in survival and the potential for prolonged disease-free survival in some patients with metastatic disease.
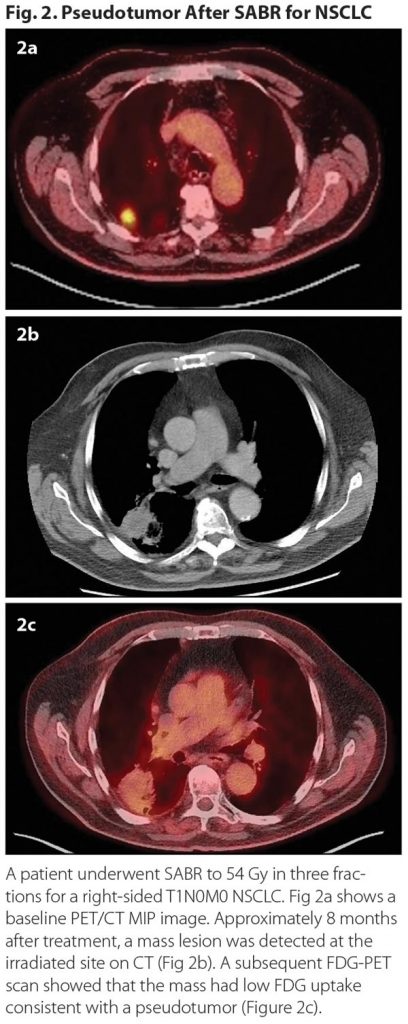
Both TKIs and immune checkpoint inhibitors have associated toxicities that influence PET -interpretation, including severe pneumonitis, which can be well visualized on FDG-PET. Changes in FDG uptake with the treatment of pneumonitis can provide objective evidence of therapeutic response (e.g., to steroids, Fig. 3) and contribute to clinical decision making for both the cancer and for treatment related toxicity. PET clinicians interpreting scans should be fully aware of the initiation of relevant systemic therapies and consider their effects on differential diagnosis. ✦
About the Authors: Prof. MacManus is with the Department of Radiation Oncology, Division of Radiation Oncology and Cancer Imaging, Peter MacCallum Cancer Centre, Melbourne, Australia, and The Sir Peter MacCallum Department of Oncology, The University of Melbourne, Melbourne, Australia. Prof. Akhurst is an associate professor with the Centre for Molecular Imaging, Division of Radiation Oncology and Cancer Imaging, Peter MacCallum Cancer Centre, Melbourne, Australia and The Sir Peter MacCallum Department of Oncology, The University of Melbourne, Melbourne, Australia.
References:
1. Mac Manus MP, Hicks RJ, Matthews JP, et al. Positron emission tomography is superior to computed tomography scanning for response-assessment after radical radiotherapy or chemoradiotherapy in patients with non-small-cell lung cancer. J Clin Oncol. 2003;21:1285-1292.
2. Murray P, Franks K, Hanna GG. A systematic review of outcomes following stereotactic ablative radiotherapy in the treatment of early-stage primary lung cancer. Br J Radiol. 2017;90:20160732.
3. Everitt S, Herschtal A, Callahan J, et al. High rates of tumor growth and disease progression detected on serial pretreatment fluorodeoxyglucose-positron emission tomography/computed tomography scans in radical radiotherapy candidates with nonsmall cell lung cancer. Cancer. 2010;116:5030-5037.
4. Konert T, Vogel W, MacManus MP, et al. PET/CT imaging for target volume delineation in curative intent radiotherapy of non-small cell lung cancer: IAEA consensus report 2014. Radiother Oncol. 2015;116:27-34.
5. Wahl RL, Jacene H, Kasamon Y, et al. From RECIST to PERCIST: Evolving Considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50 Suppl 1:122S-150S.










