By Pranshu Mohindra, MD, MBBS, DABR®, Lecia Sequist, MD, and Laurie E. Gaspar, MD, MBA
Posted: December 2017
Since the initial approval of erlotinib, an oral tyrosine kinase inhibitor (TKI), for treatment of patients with previously treated locally advanced or metastatic non-small cell lung cancer (NSCLC), multiple additional treatment agents targeting EGFR mutation are now recommended for use in clinical practice.1 Estimated median survival for patients with previously untreated EGFR-mutant positive (EGFRmt (+)) NSCLC can extend well beyond 2 years; however, this increase in longevity has been linked with an increased incidence of brain metastases (BM).2,3 While whole-brain radiotherapy (WBRT) was previously considered the standard of practice, the concern for neurocognitive side effects has led to the decreased use of WBRT in favor of stereotactic radiosurgery (SRS), as supported by phase-III trials that do not demonstrate a detriment in survival.4-6
EGFRmt (+) NSCLC provides a unique therapeutic setting where even with a diagnosis of BM, extended survival may be seen.7 A debate was conducted at the recently concluded 2017 IASLC meeting in Chicago, reviewing the pros and cons of withholding radiation therapy in patients with EGFRmt (+)-NSCLC diagnosed with BM. Key highlights from the debate presented by Dr. Lecia Sequist (Pro) and Dr. Laurie Gaspar (Con) are excerpted below.
Pro: Dr. Lecia Sequist 
1. A multi-institutional retrospective study evaluated upfront radiation (WBRT or SRS) approaches versus upfront EGFR-directed therapy approaches for these patients and showed a significant detriment in overall survival (OS) by delayed use of either of the radiation options.8 However, there are limitations in this experience, with other literature review showing mixed results:
• The presence of central nervous system (CNS)-only disease in 76% of the patients likely biased the outcomes in favor of upfront radiation.
• Also, SRS was planned only at intracranial progression, not as planned consolidation of residual disease.
• In a literature review of other institutional experiences, mixed results were observed, with 2 other studies showing survival advantage with use of radiation, 1 study showing survival advantage with TKI alone, and 3 other studies showing no significant differences, although a trend of a 4- to 7-month survival improvement with radiation was noted.
2. All published studies to date used erlotinib- or gefitinib-based therapy, which have demonstrated less CNS penetration compared to newer EGFR TKIs. Outcomes are superior in the osimertinib era.
• AURA 2 study, a phase II study evaluating use of AZD9291 (osimertinib) in EGFR and T790M mutation positive tumors after previous EGFR TKI therapy, demonstrated a 54% overall response rates (ORR) within the brain (2016 World Conference on Lung Cancer, Vienna, Austria).
• The phase I BLOOM study evaluated the use of osimertinib in patients with EGFRmt (+) leptomeningeal disease. Among 21 patients, efficacy assessments confirmed radiological response in 7 and cytological CSF clearance in 2 patients (2016 ASCO Annual Meeting, Chicago, US).
• AURA 3 study demonstrated that the ORR in brain with osimertinib in comparison with chemotherapy in patients with progression after first-line TKI therapy were 70% vs. 31%, p = 0.015 (2017 ASCO Annual Meeting, Chicago, USA). In a follow-up detailed report of this phase 3 study, analysis of 144 patients with T790M-positive advanced NSCLC who develop BM demonstrated a significant improvement in progression-free survival (PFS) favoring osimertinib as against platinum-pemetrexed chemotherapy doublet: 8.5 months vs 4.2 months (HR, 0.32; 95% CI, 0.21 to 0.49).9
• In the FLAURA study comparing osimertinib to standard therapy (erlotinib or gefitinib) in EGFRmt (+) -NSCLC, in patients with BM (n = 116), the median PFS with osimertinib versus standard therapy was 15.2 months vs. 9.6 months (HR, 0.47; 95% CI, 0.30-0.74; P = 0.0009). The rates of CNS progression were 6% versus 15%, respectively (2017 ESMO Congress, Madrid, Spain).
Bottom line: Given the risk of radionecrosis or steroid dependence from SRS or cognitive decline from WBRT, and in light of particularly encouraging outcomes from recent studies evaluating osimertinib in BM, I support use of upfront systemic therapy to offer patients an opportunity for response and thereby delay the risk of side effects from the use of radiation therapy. I also favor consideration of SRS to any significant residual CNS lesions after initial response to TKIs, a sequence and therapeutic strategy employed increasingly at most academic centers, an approach that has not been permitted in most published studies.
Con: Dr. Laurie E. Gaspar 
1. The prognosis of EGFRmut (+) BM and the time to salvage SRS/ WBRT is not as good as perceived, especially if BM occur while on TKI.
• In the Massachusetts General Hospital experience, patients with EGFRmt (+) or ALK translocation who developed BM in the setting of prior TKI therapy had worse OS than those not on TKI prior to the BM diagnosis (median OS 9m vs. 19.6 m, p < 0.001).10 Further, after cranial radiotherapy, EGFR mutation status did not impact OS.10
• In a multi-institutional retrospective database, median OS after diagnosis of BM for EGFRmt patients was 23 months (17 months for TKI treated versus 30 months for TKI-naive patients, p < 0.01). When time-dependent analysis was performed, extended survival associated with EGFRmt (+) NSCLC was only noted in TKI-naive patients relative to those who developed BM while on TKI therapy.11
• Even on the AURA 3 study, despite the 70% ORR, median PFS for patients whose disease had progressed on first-line TKI and develop CNS disease was only 8.5 months.9
• In a phase-II Japanese study using gefitinib in EGFRm-NSCLC with brain metastases, despite a 87.8% ORR, the median time on gefitinib was only 10.6 months with intracranial progression being the most common cause of withdrawal.12
2. While neurocognitive effects following WBRT are well known, there are no comparable data on the neurocognitive effects of TKI.
3. In afatinib-treated patients in the LUX-Lung 3 and LUX-Lung 6 trials, the benefit of afatinib appeared higher in patients with prior WBRT with median PFS in entire cohort ranging from 8.2 to 11 months.13
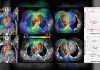
4. Results reported in the study by Magnuson et al are compelling across all prognostic subpopulations.8 This multi-institutional retrospective study evaluated upfront radiation (WBRT or SRS) approaches versus upfront EGFR-directed therapy approaches for these patients and showed a significant detriment in OS by delaying implementation of either of the radiation options. Key findings are:
• Median OS for upfront-SRS, upfront-WBRT and upfront EGFR-TKI, with SRS or WBRT at intracranial progression, were 46, 30, and 25 months, respectively, p < 0.001.
• In both radiation cohorts, 50% of patients were symptomatic at the time WBRT was initiated, compared to only 12% of patients in the EGFR-TKI cohorts.
• Even after controlling for variables that constitute the Disease Specific Graded Prognostic Assessment (DS-GPA) score7 and the EGFRm status, upfront SRS was independently associated with improved OS relative to EGFR-TKI and delayed radiation (adjusted HR, 0.39; 95% CI, 0.26 t 0.58, p < 0.001).
• Prior EGFR-TKI use and EGFR-TKI resistance mutations were exclusions, thereby suggesting the benefit of radiation was even more pronounced in the better prognostic group.
5. The biggest concern is the overall quality of life for patients with BM and the symptoms and sequelae from the metastatic intracranial burden. Bottom line: The argument for upfront radiation is especially strong for SRS, as opposed to WBRT, so why wait and let a BM get larger or more symptomatic, and not be amenable to SRS? At the University of Colorado, these patients are given upfront SRS if possible, and then proceed to TKI. If SRS is not thought to be reasonable, then the TKI is started and SRS or WBRT is deferred until progression.
Audience response: There was a lively discussion followed by an informal vote that (predictably) declared no clear winner. ✦
References
1. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) Non-Smal Cell Lung Cancer version 9.2017, Natl. Compr. Cancer Network. (2017). https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf (accessed October 21, 2017).
2. Jackman DM, Miller VA, Cioffredi LA, et al. Impact of epidermal growth factor receptor and KRAS mutations on clinical outcomes in previously untreated non-small cell lung cancer patients: results of an online tumor registry of clinical trials. Clin Cancer Res. 2009; 15:5267-5273.
3. Shin DY, Na II, Kim CH, Park S, Baek H, Yang SH. EGFR mutation and brain metastasis in pulmonary adenocarcinomas. J Thorac Oncol. 2014; 9:195-199.
4. Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: A randomised controlled trial. Lancet Oncol. 2009; 10:1037–1044.
5. Brown PD, Jaeckle K, Ballman KV, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: A randomized clinical trial. JAMA. 2016; 316:401–409.
6. Brown PD, Ballman KV, Cerhan JH, et al. Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC•3): A multicentre, randomised, controlled, phase 3 trial. Lancet Oncol. 2017; 18:1049–1060.
7. Sperduto PW, Yang TJ, Beal K, et al. Estimating survival in patients with lung cancer and brain metastases: An update of the graded prognostic assessment for lung cancer using molecular markers (Lung-molGPA). JAMA Oncol. 2017; 3:827–831.
8. Magnuson WJ, Lester-Coll NH, Wu AJ,et al. Management of brain metastases in tyrosine kinase inhibitor-naïve epidermal growth factor receptormutant non-small-cell lung cancer: A retrospective multi-institutional analysis. J Clin Oncol. 2017; 35:1070–1077.
9. Mok TS, Wu YL, Ahn MJ, AURA3 Investigators, et al., Osimertinib or Platinum-Pemetrexed in EGFR T790M-Positive Lung Cancer. N Engl J Med. 2017; 376:629–640.
10. Mak KS, Gainor JF, NiemierkoA, et al. Significance of targeted therapy and genetic alterations in EGFR, ALK, or KRAS on survival in patients with nonsmall cell lung cancer treated with radiotherapy for brain metastases. Neuro Oncol. 2015; 17:296–302.
11. Sperduto PW, Yang TJ, Beal K, et al. The effect of gene alterations and tyrosine kinase inhibition on survival and cause of death in patients with adenocarcinoma of the lung and brain metastases. Int J Radiat Oncol Biol Phys. 2016; 96:406–413.
12. Iuchi T, Shingyoji M, Sakaida T, et al. Phase II trial of gefitinib alone without radiation therapy for Japanese patients with brain metastases from EGFR-mutant lung adenocarcinoma. Lung Cancer. 2013; 82:282–287.
13. Schuler M, Wu YL, Hirsh V, et al. First-line afatinib versus chemotherapy in patients with non-small cell lung cancer and common epidermal growth factor receptor gene mutations and brain metastases. J Thorac Oncol. 2016; 11:380–390.