By Suresh Senan, MRCP, FRCR, PhD
Posted: December 2017
Improved delivery of radiotherapy has contributed to the recent changes in guidelines for patients with lung cancer. The clinical impact of some technical advances has been modest, but the cumulative effect of many developments has led to more precise treatment delivery, and has increased the confidence of clinicians to adopt new techniques. The impact of new technology is best illustrated by referring to selected clinical stages.
Early-stage Peripheral NSCLC
The poster child of new technology is image-guided stereotactic ablative radiotherapy (SABR or SBRT), which is a technique for delivering high-dose, high-precision radiation. In early-stage peripheral non-small cell lung cancer (NSCLC), 5-year in-field tumor control rates of 90% have been reported, and the introduction of SABR has been associated with improved cure rates at the population level. The superiority of SABR over conventional radiotherapy has been established in two randomized trials, results from one of which was presented at the IASLC 18th World Conference on Lung Cancer [Ball D, WCLC 2017]. SABR resulted in superior freedom from local failure (HR = 0.29, 95% CI 0.130, 0.662, P=0.002) and also longer overall survival (HR = 0.51, 95% CI 0.51, 0.911, P=0.020).
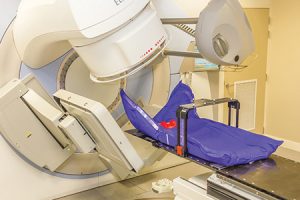
Minimal requirements for SABR planning and delivery were recently published by the European Society for Radiotherapy and Oncology, and include use of 4-D planning computed tomography (CT) scan and a standard linear accelerator with a cone-beam CT scan. Newer developments include the clinical introduction of magnetic resonance imaging-guided SABR, which is undergoing evaluation in high-risk tumors such as centrally located NSCLC. The use of protons (charged particles) was considered previously to be a promising development for treating lung tumors, due to its ability to decrease radiation doses to surrounding organs. However, the options for managing tumor motion at current proton centers is generally inferior to that available on a standard linear accelerator. At present, there are limited prospective data supporting a role for protons in early-stage NSCLC.
Locally Advanced Lung Cancer
Since the introduction of CT-based treatment planning and improved set-up protocols, concurrent chemo-radiation (CT-RT) has become established as the standard of care for most fit patients who present with locally-advanced NSCLC. Patients undergoing standard concurrent CT-RT to 60 Gy in the RTOG 0617, study achieved 5-year overall and progression free rates of 32% and 18%, respectively.1 The median overall survival of 28.7 months in this trial has also established a new benchmark. The role of intensity modulated radiotherapy (IMRT) remains a topic of debate, particularly as population studies suggest that benefits of IMRT are limited to larger central (T3-4) tumors. Results of RTOG 0617 support use of IMRT in locally-advanced NSCLC as this reduces rates of radiation pneumonitis, and was associated with a better quality of life in the first 12 months post CT-RT.
Some, but not all studies, suggested that delivery of higher radiation doses to the heart are associated with a poorer overall survival. However, other studies suggest that delivered heart doses may be a surrogate for other prognostic factors in stage III NSCLC, such as the extent and location of mediastinal nodal involvement, especially subcarinal nodes, rather than an independent predictor of outcome. The increased cardiac toxicity has also been correlated with the use of doses higher than the standard 60 Gy for CT-RT, and with schemes using non-standard fractionation schemes (>2 Gy, once daily).
Proponents of proton radiation have therefore advocated its use as a means to decrease both lung and cardiac toxicity. The number of proton centers worldwide is increasing in a roughly exponential fashion, with approximately 20 operating centers, and 53 in development. However, little consensus has been reached for using proton therapy for common types of cancer in adults. A prospective randomized trial led by the MD Anderson Cancer Center compared the use of IMRT versus proton therapy in locally advanced NSCLC, and reported no differences in treatment failures, which were defined as either grade ≥3 pneumonitis or local failure at 1 year.2 Proponents of protons have argued that the use of a newer delivery technique (intensity-modulated proton therapy) will improve outcomes, and the results of ongoing comparative trials are awaited. Treatment of mobile tumors in the lung and liver using protons remains a challenge, and only a minority (27%) of European proton and carbon ion therapy centers currently treat such tumors.3
Changing Paradigms in Locally Advanced Lung Cancer
The published results of the PACIFIC trial have called into question the previous focus on delivery of ever higher radiation doses. PACIFIC evaluated consolidation durvalumab or placebo every 2 weeks for a year, following CT-RT in patients with unselected stage III NSCLC after concurrent CT-RT to a dose of 54-66 Gy.4 Consolidation durvalumab resulted in an increase in median PFS to 16.8 versus 5.6 months (HR 0.52) with the differences in PFS sustained at 12- and 18-month landmarks. Durvalumab also resulted in a superior median time to death or distant metastases (23.2 vs 14.6 months; P < .001), and little increase in grade 3/4 treatment related toxicity. The above findings indicate that the addition of durvalumab consolidation to standard radiation doses combined with two cycles of platinum-containing chemotherapy, is sufficient to improve both local and distant tumor control. This, in turn, raises the question whether the focus of radiation research should simply be to limit radiation doses to 60 Gy, while further optimizing the integration of immune-oncology and other systemic approaches into CT-RT of stage III NSCLC. ✦
References
1. Bradley JD, Hu C, Komak RU, et al. Long-term results of RTOG 0617: A randomized phase 3 comparison of standard dose versus high dose conformal chemoradiation therapy +/- cetuximab for stage III NSCLC. J Am Coll Radiol. 2017:99, S105 (suppl)
2. Liao Z, Lee J, Komaki R, Gomez D, O’Reilly M, Allen P, et al. Bayesian randomized trial comparing intensity modulated radiation therapy versus passively scattered proton therapy for locally advanced non-small cell lung cancer. J Clin Oncol. 2016;34 suppl 15:8500.
3. Weber DC, Abrunhosa-Branquinho A, Bolsi A, et al. Profile of European proton and carbon ion therapy centers assessed by the EORTC facility questionnaire. Radiother Oncol. 2017;124:185-189.
4. Scott J. Antonia SJ, Villegas A, Davey Daniel D, et al. Durvalumab after chemoradiotherapy in stage III non–small-cell lung cancer. N Engl J Med. 2017 Sep 8. doi: 10.1056/ NEJMoa1709937. [Epub ahead of print]











