By Brendon Stiles, MD, and Drew Moghanaki, MD, MPH
Posted: June 24, 2020
Annual low-dose computed tomography (LDCT) detects more early-stage lung cancers and saves lives by preventing death in people who develop lung cancer. The recent report on the long-term follow-up of patients in the National Lung Screening Trial (NLST) makes a powerful argument against overdiagnosis and lead time bias.1 Despite screening for only the first two years of the study, after 11 years of follow-up, the cohort that underwent LDCT screening continued to have reduced lung cancer‒related mortality, suggesting that screening indeed leads to better cure rates. The recent publication of the NELSON trial should also re-energize screening efforts.2 Similar to the NLST trial, patients who underwent LDCT screening in NELSON had a 24% decreased risk of dying from lung cancer compared to patients in the control group.2,3 Using a volume-based approach, only 2.1% of screening exams required further workup, and only 1.2% of patients had a false-positive test over all screening rounds.
These beneficial effects must, of course, be balanced by the potential for harm of screening to patients ultimately not found to have lung cancer. Fortunately, rates of major complications from interventions in such patients are low, less than 4 in 10,000.2 However, this statistic often gets lost in simple graphic charts, which typically include all complications related to treatment of screen-detected lung cancers as complications of screening itself. That narrative, along with the long-standing nihilism associated with a diagnosis of lung cancer, have served to weaken enthusiasm for LDCT screening among patients and practitioners and have contributed to low utilization of lung cancer screening, potentially jeopardizing tens of thousands of lives.
Less-Invasive Lung-Sparing Techniques
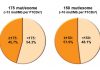
Although tremendous work is underway to change the general narrative of lung cancer screening, physicians must also carefully consider how best to treat screen-detected lung cancers to further optimize survival and quality of life in these patients. As the majority of these screened tumors are early-stage cancers, the responsibility will generally fall to surgeons and radiation oncologists. Regarding surgery, patients with screen-detected cancers would seem to be optimal candidates for minimally invasive surgery and for parenchyma–sparing, limited resections, either wedge resection or segmentectomy. Minimally invasive surgery, either thoracoscopic or robotic assisted has been associated with fewer complications and decreased length of hospital stay than traditional open thoracotomy.4,5 Although only 30% of patients with lung cancer in the NLST underwent minimally invasive surgery, the rates of uptake have proven much higher in publications from more recent surgical trials and databases such as CALGB 140503 (80%) and the Society of Thoracic Surgeons General Thoracic Surgery Database (62%). Additionally, the Dutch Lung Cancer Screening Trial, in which 84% of patients underwent minimally invasive surgery, demonstrated that such an approach should be the rule, rather than the exception for screen-detected cancers. In our previous review of the NLST dataset, we demonstrated that rates of total complications were lower with minimally invasive surgery than with thoracotomy, 27% versus 36% (p = 0.02), emphasizing the need for this approach in the modern era.6 Similarly, although we still await results of randomized trials evaluating lobectomy versus limited resection for clinical stage I lung cancers (CALGB 140503 and JCOG 0802), it would seem logical that some screen-detected cancers are good candidates for limited resection. This, of course, depends on careful staging and upon surgical expertise. It is important to note that 26% of patients in the NLST were pathologically upstaged at surgery.6 However, limited resection was performed in 16% of patients with lung cancer in the NLST. This is lower than the 20% to 31% rates reported in other databases such as the STS General Thoracic Surgery Database, the National Cancer Database, and the SEER-Medicare database. However, in our review of the NLST data, patients who underwent limited resection had fewer complications than those who underwent lobectomy (223% vs. 2%, p = 0.05), and limited resection was associated with fewer complications on multivariable analysis (OR 0.54, CI [0.34, 0.87]).6 This increased safety did not come at the expense of decreased oncologic efficacy with limited resection. Five-year OS was identical for patients with stage I disease who underwent lobectomy or limited resection (77% vs. 77%, p = 0.889). Similarly, the I-ELCAP investigators have reported excellent long-term survival with limited resection of screen-detected lung cancers.7 It should, therefore, be clear that screen-detected lung cancer can be cured with surgery. Surgery will only get safer, with more emphasis on patient-reported outcomes and on long-term quality of life, issues of critical importance to populations of patients considering cancer screening.
SBRT: Improving Survival
In addition to surgical improvements, stereotactic body radiation therapy (SBRT) is an increasingly viable alternative to surgery and may be considered as a local treatment option in some screened patients. SBRT was largely unavailable when the NLST trial was conducted, but today it offers an option that is currently accepted as the standard of care in multiple evidence-based guidelines for patients whose disease is medically inoperable. SBRT may also offer a safer alternative to patients diagnosed with screen-detected lung cancers, particularly older patients who have been demonstrated to have lower periprocedural mortality with SBRT than with surgery.8
Although representing only a small proportion (3.6%) of screen-detected cancers in the I-ELCAP prospective cohort study, patients treated with SBRT experienced a 90% 15-year lung cancer‒specific survival rate, not statistically different from that of patients undergoing surgery.9 In larger studies, outcomes with SBRT have consistently demonstrated greater than 90% primary tumor control and lung cancer‒specific mortality rates that are similar to those reported with surgery.
Although these data have been encouraging, most of the reports have been limited by retrospective study design, small cohorts, and short median duration of follow-up. However, prospective trials of patients with resectable disease have also shown excellent local control and 3-year survival rates over 75%. Additionally, the pooled results of two prospective randomized trials, although underpowered to make an adequate comparison with survival after surgery, clearly showed that select patients with operable disease may have outstanding survival when treated with SBRT, with 95% of patients alive at 3 years.10 Although these studies failed to adequately accrue enough patients for statistical power, the ongoing STABLE-MATES and VALOR trials that were activated in 2017 continue to enroll and in the future will help us better understand the suitability of SBRT as an alternative to surgery for patients with resectable disease. Until the final results of these phase III studies are reported, the availability of SBRT can at least help clinicians better select patients for surgery in order to mitigate risk in those who present with advanced comorbidities at diagnosis.
In conclusion, treatment options for patients with screen-detected lung cancer have evolved since the NLST first began enrolling patients in 2002. Minimally invasive surgical techniques have improved surgical outcomes. The option of lung-sparing techniques including sublobar resection and SBRT are now more widely available and may help to preserve long-term pulmonary function without sacrificing survival or quality-of-life. The availability of these distinct treatment options will help clinicians make careful decisions that optimize the benefits of early detection and minimize the risks of treatment in those who are diagnosed with screen-detected lung cancer.
References:
1. National Lung Screening Trial Research Team, et al. Lung Cancer Incidence and Mortality with Extended Follow-up in the National Lung Screening Trial. J Thorac Oncol. 2019;14(10):1732-1742.
2. de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med. 2020;382(6):503-513.
3. NationalLung Screening Trial Research Team, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409.
4. Lim E, Tatchelor T, Dunning J, et al. PL02.06 In Hospital Clinical Efficacy, Safety and Oncologic Outcomes from VIOLET: A UK Multi-Centre RCT of VATS Versus Open Lobectomy for Lung Cancer. J Thorac Onc. 2019;14(10):S6.
5. Paul S, Altorki NK, Sheng S, et al. Thoracoscopic lobectomy is associated with lower morbidity than open lobectomy: a propensity-matched analysis from the STS database. J Thorac Cardiovasc Surg. 2010;139(2):366-378.
6. Kamel MK, Lee B, Harrison S, et al. Do the surgical results in the National Lung Screening Trial reflect modern thoracic surgical practice? J Thorac Cardiovasc Surg. 2019;157(5):2038-2046.
7. Altorki NK, Yip R, Hanaoka T, et al. Sublobar resection is equivalent to lobectomy for clinical stage 1A lung cancer in solid nodules. J Thorac Cardiovasc Surg. 2014;147(2):754-762; Discussion 762-764.
8. Stokes WA, Bronsert MR, Meguid RA, et al. Post-Treatment Mortality After Surgery and Stereotactic Body Radiotherapy for Early-Stage Non-Small-Cell Lung Cancer. J Clin Oncol. 2018;36(7):642-651.
9. Berlin E, Buckstein M, Yip R, et al. Definitive Radiation for Stage I Lung Cancer in a Screened Population: Results From the I-ELCAP. Int J Radiat Oncol Biol Phys. 2019;104(1):122-126.
10. Chang JY, Senan S, Paul MA, et al. Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Oncol. 2015;16(6):630-637.
About the Authors:
Dr. Stiles is an associate professor of Cardiothoracic Surgery, Weill Cornell Medicine, New York-Presbyterian Hospital.
Dr. Moghanaki is an associate professor in the Department of Radiation Oncology, Emory University School of Medicine, and section chief in the Department of Radiation Oncology, Atlanta VA Medical Center.
ILCN Welcomes Dr. Stiles to Editorial Planning Group
Dr. Brendon Stiles is the newest addition to ILCN’s Editorial Planning Group. A thoracic surgeon at New York-Presbyterian Hospital and an associate professor of cardiothoracic surgery at Weill Cornell Medicine, Dr. Stiles is also very active on social media. An extremely dedicated IASLC volunteer, follow Dr. Stiles on Twitter (@BrendonStilesMD) for live updates from various IASLC activities and meetings, as well as for insights on patient research and advocacy.