By Enza Esposito Nguyen, DNP, RN, ANP-BC
Posted: February 12, 2020

Although we continue to see many immunotherapy clinical trials mature and deliver marvelous improvements in PFS and OS in lung cancer and many other malignancies, managing some of the adverse events (AEs) of immunotherapy has become a unique challenge. This is most evident when patients receiving immunotherapy present outside of the cancer center, for example to an emergency department (ED). This has led to the identification of a clinical chasm among non-oncology providers in community cancer centers. This clinical gap is now well documented in the emergency and critical care medicine literature.1,2,4
The purpose of the Doctor of Nursing Practice (DNP) project was to educate and facilitate the adoption of evidence-based guidelines (National Comprehensive Cancer Network V 1.2018) in the management of checkpoint inhibitor-related AEs by nononcology providers at Providence St. Joseph in Orange, California, a community hospital. As a result, the study questions included: What is the baseline knowledge about checkpoint inhibitors, their AEs, and their management by non-oncology providers? What would be the most effective way to impart this information to non-oncology providers? Can we examine the effects of this new knowledge on the clinical outcomes of patients receiving immunotherapy who are seen in the ED and admitted to the hospital for suspected AEs?
Methods
During this project, educational in-services were provided to non-oncology providers on the newly published guidelines. A knowledge pretest and posttest assessed changes from baseline understanding, and chart audits were completed to evaluate success of knowledge dissemination on patient treatment. Lastly, de-identified data from quality improvement audits through the electronic medical records were reviewed to assess patient outcomes. Targeted 7- to 10-minute micro-teaching sessions were provided for nurses in various non-oncology areas including the ED, medical-telemetry, and the intensive care units. Similar concise micro-teaching education was also provided for physicians in the ED; physician education focused on the pharmacokinetics of immunotherapy, commonly seen AEs, and newly released management guidelines. These micro-teaching sessions consisted of one to seven providers at a time and included the use of a laptop or a ringed booklet with PowerPoint slides as audiovisual aides. A knowledge pretest/posttest was administered to the nurses and physicians.
All data from the pre/posttest knowledge questionnaire were analyzed using SPSS (version 24) statistics software. Data were checked for accuracy. Descriptive statistics were used to illustrate the demographic characteristics of providers who completed the knowledge tests at each time point. Total scores were calculated, and phi coefficients were calculated to assess the relationship between baseline and post-education knowledge for each item. Nursing data from all units and specialties were reported under “all RNs” in the result section, and physician data were reported separately.
Results
Between October and December 2018, 73 (66%) nurses and 16 (72%) physicians from the ED received the in-service. This met the goal to educate most of this critical frontline staff. Additionally, 18 nurses from intensive care, 13 nurses from oncology, nine nurses from medical-telemetry, and 12 from general surgery participated in the microteaching in-services for inpatient nursing staff.
Nurses
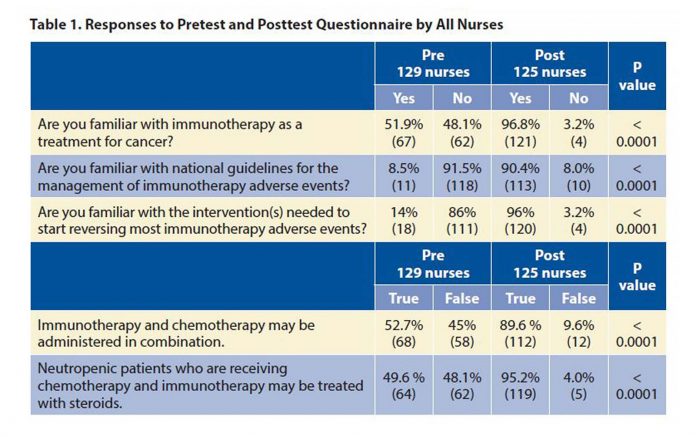
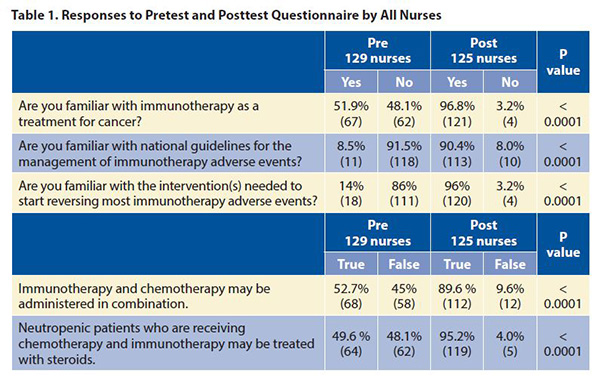
The results (Table 1) reflect increased knowledge for all nurses between pre- and posttest (125 nurses). For each of the five questions, the percentage of nurses who correctly responded to the item significantly increased at posttest (p < 0.001). Baseline nurse knowledge of interventions to reverse checkpoint inhibitor AEs was low prior to the microteaching; 14% correctly responded compared to 96% after education.
Physicians
Table 2 reports the results for the ED physicians (16 physicians). At baseline, physician knowledge scores were higher than baseline knowledge for all nurses. For example, at baseline, for the question “Are you familiar with the intervention needed to start reversing most immunotherapy adverse events,” 21.4% of ED physicians answered “yes” compared to 14% for all nurses. On only two questions did physicians increase their knowledge significantly post-teaching. One was the question mentioned previously, which featured a significant increase in knowledge following the micro-teaching in-service (p < 0.0001). The other item with a significantly increased proportion of correct responses was being familiar with national guidelines for the reversal and management of AEs due to checkpoint inhibitors (p = 0.004).
Discussion/Implications
Nurses more than physicians demonstrated limited baseline understanding of the signs and symptoms of immunotherapy AEs. Interestingly, many nurses and physicians when asked to “name some immunotherapy adverse events” wrote down AEs associated with chemotherapy. This is consistent with other publications that suggest similar deficits among providers.1,4
Knowledge among physicians was higher during baseline assessment, with pretest results demonstrating means between 14% and 85%. This could be attributed to a couple of factors. First, there has been more recent publications in the emergency department literature regarding checkpoint inhibitors, AEs, and their assessment and management, as appraised in our literature review. Second, some of these physicians may have previously attended the introductory educational in-service with the institution of immunotherapy identifi cation cards as part of phase 1, which was provided in Summer 2017.
Although the project was conducted over a short period of time, which did not allow for training of all nursing staff members and all specialists regarding IO AE management,4 the project was successful in that it increased the knowledge base of the emergency frontline staff about immunotherapy, its complicated AEs, and how to reach out to the oncology team and manage these AEs more confidently in a community tertiary center. The project also revealed additional gaps in care that were readily addressed. ✦
About the Author: Dr. Nguyen was a Thoracic Oncology Nurse Practitioner at Providence St Joseph Hospital in Orange at the time this doctoral project was conducted.
References:
1. Hryniewicki AT, Wang C, Shatsky RA, Coyne CJ. Management of immune checkpoint inhibitor toxicities: A review and clinical guideline for emergency physicians. J Emerg Med. 2018;55(4):489-502.
2. Kroschinsky F, Stölzel F, von Bonin S, et al. New drugs, new toxicities: Severe side effects of modern targeted and immunotherapy of cancer and their management. Crit Care. 2017;21(1):89.
3. National Comprehensive Cancer Network. Management of immunotherapy-related toxicities (Version 5.0 2018). nccn.org/professionals/physician_gls/pdf/immunotherapy.pdf. Published 2018. Accessed August 15, 2019.
4. Wang DY, Salem YE, Cohen JV, et al. Fatal toxic effects associated with immune checkpoint inhibitors: A systematic review and meta-analysis. JAMA Oncol. 2018;4(12):1721-1728.