Patients with lymph node metastasis would benefit most from adjuvant therapy, and TKIs provide a more appropriate choice for the EGFR mutant group.
By Si-Yang Liu, MD, and Yi-Long Wu, MD
Posted: November 12, 2019


In the twentieth century, adjuvant chemotherapy became the standard of care for resected NSCLC based on several clinical trials including IALT, JBR.10, ANITA, and a meta-analysis of individual patient data from the LACE trial. Adjuvant chemotherapy increased overall survival (OS) by 5% at 5 years, and resected NSCLC was considered a “curable disease.” The question raised was whether these patients with resected NSCLC could really be cured. According to the Eighth Edition Lung Cancer Stage Classification, 5-year OS in resected NSCLC ranged from 90% for stage IA disease down to 41% for pathologic stage IIIA disease.1 As for patients with stage II to IIIA disease with lymph node metastasis, 5-year OS was only 40% to 50%, implying that more than half of these patients could not be cured.1 This is a very important point, in that the survival of those with so-called “curable disease” is heterogeneous. Th ere is a huge medical need to improve the long-term survival of patients whose cancers are destined to recur after surgery.
Patient Selection for Adjuvant EGFR TKIs
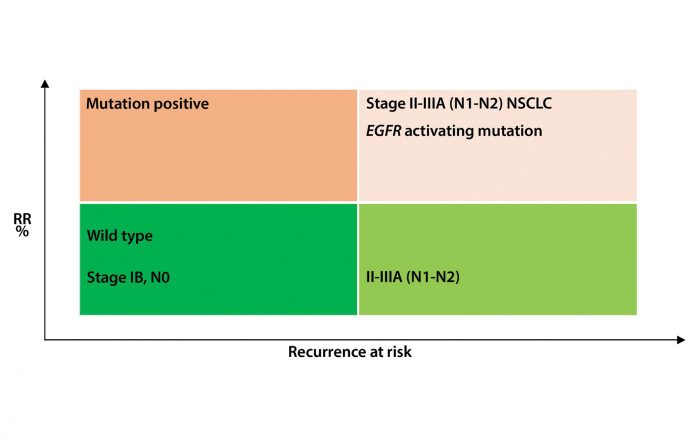
In the adjuvant chemotherapy era, NSCLC was considered a single disease, so most trials were designed for all comers. BR.19, the first trial to evaluate an EGFR TKI (gefitinib) in the adjuvant setting, and the subsequent RADIANT trial, which compared erlotinib to placebo, were not designed specifically for patients with EGFR mutations. Thus, it is no surprise that these two adjuvant TKIs failed to show meaningful benefits.2,3 Since the publication of the phase III randomized controlled trial IPASS in 2009, NSCLC, particularly in East Asia, has been classified as EGFR mutant and EGFR wild type. Along with the use of small-molecule TKIs, significantly superior survival benefits have been achieved in select patients, with advanced EGFR-mutated NSCLC.4,5 As a result, EGFR TKIs have successfully established their first-line treatment position in this subgroup, replacing chemotherapy upfront.6 Extrapolating our knowledge from advanced NSCLC to so-called curable NSCLC, we know that N1 to N2 NSCLCs have the highest risk of recurrence and are more likely to respond to EGFR TKIs in patients harboring an EGFR mutation (Figure). As a result, we hypothesized that EGFR TKIs might play an important role in the adjuvant setting in such patients. One of the most important points is that the patients with stage I disease had lower recurrence rates and higher 5-year survival (~80%). So it was rational to exclude patients with resected stage IB NSCLC from automatic enrollment onto adjuvant clinical trials (Figure).
Given these facts, we conducted an ADJUVANT phase III clinical trial for patients with actionable EGFR mutations, which only targeted N1 and N2 disease.
Dose and Schedule
The distinguishing design feature of the ADJUVANT trial was a direct comparison of adjuvant TKIs with vinorelbine plus cisplatin instead of comparing TKIs with placebo after chemotherapy, as evaluated in the BR.19 and RADIANT trials. Unsurprisingly, compliance with adjuvant TKIs (95.5%) was better than that with chemotherapy (78.4%) in our ADJUVANT trial. This means that patients receiving adjuvant TKIs were more likely to complete treatment than patients receiving standard chemotherapy. Another issue was how long to treat these patients. In addition, we raised the question of whether disease-free survival (DFS) would be a reasonable endpoint. Would it be a surrogate for OS?
Based on the data from TNM staging, the median DFS for patients with N1- to N2-positive disease ranged between 9.0 and 21.0 months, so the duration of EGFR-TKIs was set up as 24 months to best reduce recurrence.7 However, based on observations from the SELECT study, future research directions should include a straight phase II trial evaluating erlotinib in the adjuvant setting, the length of therapy’s effect on outcomes, and optimal duration. Trials testing longer treatment durations, such as ADAURA (adjuvant osimertinib vs placebo after chemotherapy), are underway.8,9
Cure Versus Extended Response
Because OS has been always considered the primary endpoint for most clinical trials, researchers may question whether adjuvant TKIs are able to improve cure rates or whether they just delay recurrence. The design of ADJUVANT is different from RADIANT, and the hypothesis of the two trials designs is different. The ADJUVANT study was created to test whether an EGFR TKI might be a viable treatment alternative to chemotherapy in the adjuvant setting, specifically in EGFR mutant (+) NSCLC. In this situation, we believed that using DFS as the primary endpoint was rational. The U.S. Food and Drug Administration has stated that a prolonged delay in the development of metastatic disease is an objective and a clinically relevant outcome and that agents can be approved based on metastasis-free survival (MFS) if substantial effects on this endpoint are demonstrated and the safety profile is acceptable.10 In addition, after adjuvant gefitinib or erlotinib, patients with disease recurrence still have the opportunity to be re-challenged with TKIs. And the median duration of treatment approximates the progression-free survival in a de novo advanced EGFR-mutant population.8,11 Furthermore, several novel treatments such as third-generation TKIs have the opportunity to provide survival benefits after progression. Consequently, whether OS is the most appropriate endpoint remains an open question, and DFS is considered by many a suitable surrogate endpoint.12
In more recent times, in advanced NSCLC, the application of EGFR-TKIs such as dacomitinib has significantly prolonged OS.13 In fact, virtually all patients with EGFR-positive NSCLC live longer than they had previously, in both the early- and late-disease settings. So in the early-disease setting it is important to delay recurrence and reduce adverse events so that patients have a better quality of life.14 This is in line with FDA guidance on MFS.
On the other hand, adjuvant trials for early-stage NSCLC take a long time to complete. The BR.19 and RADIANT trials took more than 10 years to report. The ALCHEMIST study is another ongoing adjuvant setting trial first initiated in 2014 by the National Cancer Institute and is still enrolling patients with EGFR mutations. Based on the trial design, the timeframe for accrual will be at least 10 years before we can assess the primary endpoint of OS.
Conclusions
The treatment paradigm for NSCLC has dramatically changed over the past 10 years. New EGFR TKIs such as dacomitinib and osimertinib have been approved. When a trial is destined to last 10 or more years, one must consider whether the results are still clinically meaningful by the time the trial has been completed.
However, we still see a substantial portion of patients in the ADJUVANT trial who experience relapse. One question is how to select populations more precisely for adjuvant treatment. Learning from the experience of minimal residual disease in leukemia, monitoring circulating tumor DNA (ctDNA) in the plasma as a treatment marker may be a potential strategy in the adjuvant setting. From the evolutionary perspective, we might monitor ctDNA dynamically so that the duration and ideal termination of adjuvant TKIs could be precisely determined. In patients with “wild-type” NSCLC, where EGFR mutations and other oncogenic drivers are not present, immunotherapy has become an established component of treatment in advanced disease and is being evaluated increasingly in the perioperative setting. Recently, nivolumab was approved as adjuvant treatment for resected melanoma based on the improved relapse-free survival. For personalized adjuvant treatment in the future, we need to identify patients precisely and match the appropriate treatment with the appropriate patient. ✦
About the Authors: Dr. Liu is with Guangdong Lung Cancer Institute, Guangdong Provincial Key Laboratory of Translational Medicine in Lung Cancer, Guangdong Provincial People’s Hospital and Guangdong Academy of Medical Sciences, Guangzhou, China. Dr. Wu is tenured Professor of the Guangdong Provincial People’s Hospital and Guangdong Academy of Medical Sciences and an honorary director of Guangdong Lung Cancer Institute, in China.
References:
1. Detterbeck FC, Boff a DJ, Kim AW, et al. The Eighth Edition Lung Cancer Stage Classification. Chest. 2017;151(1):193-203.
2. Goss GD, O’Callaghan C, Lorimer I, et al. Gefitinib versus placebo in completely resected non-small-cell lung cancer: results of the NCIC CTG BR19 study. J Clin Oncol. 2013;31(27):3320-3326.
3. Kelly K, Altorki NK, Eberhardt WE, et al. Adjuvant Erlotinib Versus Placebo in Patients With Stage IB-IIIA Non-Small-Cell Lung Cancer (RADIANT): A Randomized, Double-Blind, Phase III Trial. J Clin Oncol. 2015;33(34):4007- 4014.
4. Herbst RS, Morgensztern D, Boshoff C. The biology and management of non-small cell lung cancer. Nature. 2018;553(7689):446-454.
5. Hirsch FR, Scagliotti GV, Mulshine JL, et al. Lung cancer: current therapies and new targeted treatments. Lancet. 2017;389(10066):299-311.
6. Mok TS, Wu YL, Th ongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947-957.
7. Zhong W-Z, Wang Q, Mao W-M, et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for stage II–IIIA (N1–N2) EGFR -mutant NSCLC (ADJUVANT/CTONG1104): a randomised, open-label, phase 3 study. Lancet Oncol. 2018;19(1):139-148.
8. Pennell NA, Neal JW, Chaft JE, et al. SELECT: A Phase II Trial of Adjuvant Erlotinib in Patients With Resected Epidermal Growth Factor Receptor-Mutant Non-Small-Cell Lung Cancer. J Clin Oncol. 2019;37(2):97-104.
9. Romero D. Adjuvant TKIs — a long-term matter. Nat Rev Clin Oncol. 2019;16(2):67.
10. Blumenthal GM, Pazdur R. Approvals in 2018: a histology-agnostic new molecular entity, novel end points and real-time review. Nat Rev Clin Oncol. 2019 Jan 22. [Epub ahead of print].
11. Oxnard GR, Janjigian YY, Arcila ME, et al. Maintained sensitivity to EGFR tyrosine kinase inhibitors in EGFR-mutant lung cancer recurring after adjuvant erlotinib or gefitinib. Clin Cancer Res. 2011;17(19):6322-6328.
12. Mauguen A, Pignon JP, Burdett S, et al. Surrogate endpoints for overall survival in chemotherapy and radiotherapy trials in operable and locally advanced lung cancer: a re-analysis of meta-analyses of individual patients’ data. Lancet Oncol. 2013;14(7):619-626.
13. Mok TS, Cheng Y, Zhou X, et al. Improvement in Overall Survival in a Randomized Study That Compared Dacomitinib With Gefitinib in Patients With Advanced Non-Small-Cell Lung Cancer and EGFR-Activating Mutations. J Clin Oncol. 2018;36(22):2244-2250.
14. Wu Y-L, Zhong W-Z. Adjuvant therapy for resected EGFR-mutant non-small-cell lung cancer – Authors’ reply. Lancet Oncol. 2018;19(3):e127.
15. Ng TL, Camidge DR. Lung cancer’s real adjuvant EGFR targeted therapy questions. Lancet Oncol. 2018;19(1):15-17.










