
By Anne-Claire Toffart, MD, PhD, and Jean-François Timsit, MD, PhD
Posted: April 1, 2019

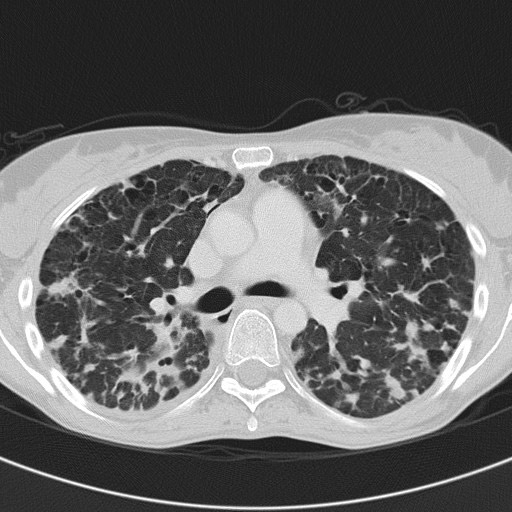
Survival rates for patients with lung cancer who were admitted into the intensive care unit (ICU) have improved during the past 2 decades. In recent studies, ICU mortality for those patients admitted on an unscheduled basis was 30% to 40%.1,2 This improved ICU survival rate is due to a better understanding of organ dysfunction and to breakthroughs in lung cancer treatment such as targeted therapies and immune checkpoints inhibitors. In addition, it is possible that earlier admission and more careful selection of patients who would benefit most from an ICU admission also have contributed to improved ICU survival rates. Nevertheless, among patients with hematologic and solid tumors, patients with lung cancer often have the poorest prognosis, which often leads to a refusal of ICU admission or stigmatization during the admittance process. Although stigmatization after ICU admission was previously an issue, the past 10 years or so has shown great improvement in the understanding of ICU staff and care specialists regarding therapeutic benefits and side effects of more modern treatments. Perhaps this improved understanding is not as prevalent in other parts of the world but, in the experience of the authors, stigmatization of patients is more frequently seen (and, therefore, more important) prior to ICU admission.

Oncologists and supportive care specialists should remember the objectives of treatment for critically ill patients with cancer in the ICU: to discharge the patient from the ICU and the hospital with an acceptable quality of life and, if warranted, to provide benefit from further cancer therapy (Figure). Anticipation of issues associated with ICU admission, as well as a close alliance between the oncologist and the intensive care specialists are the two keys to the success of a patient-centered healthcare plan in life-threatening situations.

Establishing a Patient-Centered Healthcare Plan
Each individual patient is central to the decision-making process about ICU admission. Patient wishes or advance directives are obviously extremely important to this process. In the context of intensive care, the patient and/or relatives are often unable to express coherent desires regarding his or her overall treatment goals or overall healthcare plan.3 End-of-life (EOL) discussions between the patient and the primary oncologist are of upmost importance because the patient is not always aware of his own care plan, nor is the appointment of legal representatives for decision making and the creation of advance directives systematic. Any patient wishes expressed during the EOL discussion should be written clearly in the medical file to be easily accessible in case of emergency. In a prospective study, early EOL discussions were associated with less aggressive care and greater use of hospice at EOL.4
Identifying the Necessary Level of Support, Bolstering Survival
Factors associated with survival were related to patient characteristics, cancer history, and acute disease.5 For example, patients with a poor performance status (PS score higher than 2) had poor survival. Both the overall treatment plan and treatment response are probably more important than metastatic status. This is particularly true for patients who are eligible for targeted therapy6 or who are responding to immune checkpoint inhibitors. Finally, patients with cancer must be admitted to ICU with few organ failures. Patients with no organ dysfunction but physiologic disturbances could also be admitted in order to avoid late ICU admission (condition associated with higher mortality).7 Uses of invasive mechanical ventilation or vasopressors are known to be associated with ICU mortality.
Clarification of a patient’s code status is necessary at the time of admission.8 In patients admitted with a full-code status, the decision-making process is similar to that of other patients in the ICU without malignancy. ICU trial consists of unlimited ICU support for a limited time period. Trials of ICU care lasting 1 to 4 days may be sufficient for patients with poor-prognosis solid tumors.9 Limited support can also be offered at ICU admission; for example, respiratory support or hemodynamic failure support. Admission policy should be explained to the patient and/or relatives. After 3 days of ICU care, a discussion regarding the intensity of care is strongly recommended for each patient. Oncologists should continue to participate in the decision-making process during the patient’s ICU stay and should be present for all patient/caregiver discussions. ✦
About the Authors: Dr. Toffart is associate professor in the thoracic oncology unit, Grenoble Alpes Teaching Hospital, France. Dr. Timsit is professor in the Medical and Infectious Diseases ICU, Bichat-Claude Bernard Hospital, APHP, France.
References:
1. Soubani AO, Ruckdeschel JC. The outcome of medical intensive care for lung cancer patients: the case for optimism. J Thorac Oncol. 2011; 6: 633-638.
2. Ostermann M, Ferrando-Vivas P, Gore C et al. Characteristics and Outcome of Cancer Patients Admitted to the ICU in England, Wales, and Northern Ireland and National Trends Between 1997 and 2013. Crit Care Med. 2017; 45: 1668- 1676.
3. Rigaud JP, Large A, Meunier-Beillard N, et al. What are the ethical aspects surrounding intensive care unit admission in patients with cancer? Ann Transl Med. 2017;5(Suppl 4):S42.
4. Mack JW, Cronin A, Keating NL, et al. Associations between end-of-life discussion characteristics and care received near death: a prospective cohort study. J Clin Oncol. 2012;30(35):4387-4395.
5. Toffart AC, Minet C, Raynard B, et al. Use of intensive care in patients with nonresectable lung cancer. Chest. 2011;139(1):101-108.
6. Toffart AC, Dhalluin X, Girard N, et al. Patients with advanced lung cancer harboring oncogenic mutations should be admitted to intensive care units. Intensive Care Med. 2015;41(1):164-165.
7. Thiery G, Azoulay E, Darmon M, et al. Outcome of cancer patients considered for intensive care unit admission: a hospital-wide prospective study. J Clin Oncol. 2005;23(19):4406-4413.
8. Azoulay E, Soares M, Darmon M, et al. Intensive care of the cancer patient: recent achievements and remaining challenges. Ann Intensive Care. 2011;1(1):5.
9. Shrime MG, Ferket BS, Scott DJ, et al. Time-Limited Trials of Intensive Care for Critically Ill Patients With Cancer: How Long Is Long Enough? JAMA Oncol. 2016;2(1):76-83.










