By Richard Booton, MD, PhD, FRCP
Posted: April 1, 2019

The symptomatic presentation of lung cancer is typically associated with advanced disease and poor survival. Screening asymptomatic at-risk individuals using low-dose CT (LDCT) reduces lung cancer–specific mortality by 20% to 26%,1 but challenges remain in ensuring participation of the most at-risk populations, such as current smokers or those of lower socioeconomic status. Travel to hospital sites is recognized as a key barrier to access; screening among this at-risk population and reducing these barriers are critical to the successful implementation of LDCT screening.
One-Stop Shop: Cessation Advice, LDCT Scanning, and Scan Interpretation
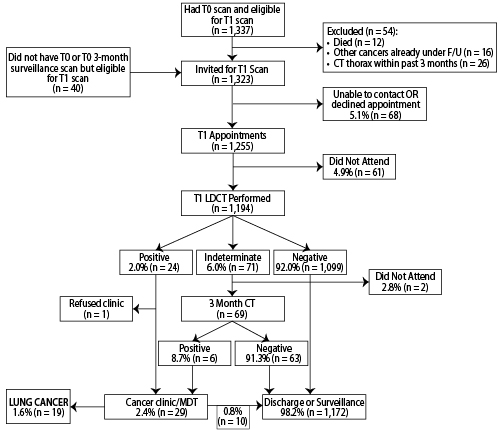
A pragmatic, community-based pilot was designed around the concept of a one-stop lung health check, located next to local shopping centers, to minimize barriers to participation by reducing travel and increasing convenience and service accessibility (Figure). Eversmokers aged 55 to 74 years registered by participating general practitioners were invited and assessed for symptoms, spirometry, and 6-year lung cancer risk using PLCOm2012 and were provided with brief, non-judgemental smoking-cessation advice where appropriate. Participants with PLCOm2012 risk score of 1.51% or greater were offered immediate LDCT scanning on a co-located scanner, and imaging was interpreted by radiologists with a specialist interest in thoracic oncology according to modified British Thoracic Society Guidelines for the Investigation and Management of Pulmonary Nodules. Scan reports were categorized as negative, indeterminate, or positive. Indeterminate results required a community-based 3-month followup scan, and positive scans required an immediate assessment at a lung cancer clinic within a regional cardiothoracic center. Participants eligible for LDCT scanning underwent a baseline scan (T0) and a single annual scan (T1).
[epub ahead of print].
Between June and August 2017, 1,194 participants underwent their T1 community-based scan, confirming a 90% adherence to LDCT screening. A negative scan was identified for 92%, and a positive scan was identified for 2.5% of participants; 5.9% of participants had indeterminate scans (6 participants had positive scans at 3 months). Of 29 participants referred for further evaluation (2.4%), 19 were diagnosed with lung cancer, representing a false-positive rate of 34.5% (0.8% of all T1 participants). The incidence of lung cancer at T1 was 1.6%, 79% had stage I-II disease, and curative-intent treatment was provided in 78.9% (surgery 47%, stereotactic ablative radiotherapy 26%, and radical radiotherapy 5%). One participant received surgery for granulomatous disease; there were no deaths at 90 days. The false-negative rate for T0 was 0.4%, with a negative predictive value of 99.6%, sensitivity of 89.4%, and specificity of 97.1%. Overall (T0 + T1), the benign surgical resection rate was 2.5%.3
Saving Lives, Saving Money
This pilot was undertaken in low-income areas of Manchester, United Kingdom, and it used a “Lung Health Check” design to facilitate uptake of a targeted lung cancer screening program. Attendees could be ranked according to degree of deprivation in small areas of England, using domains that included income, employment, education, health, crime, environment, and barriers to housing, from 1 (most deprived) to 32,844 (least deprived). Seventy-five percent of attendees were ranked in the lowest deprivation quintile, and screening adherence was high. Throughout both screening rounds, we identified one lung cancer for every 23 scans performed. Approximately 80% of lung cancers were identified at an early stage and underwent high rates of curative-intent surgery, with low false-positive rates and low benign surgical resection rates. An ultra-conservative cost-effectiveness analysis of the pilot suggested an incremental cost-effectiveness ratio of £10,069 per quality-adjusted life year, well within current National Institute for Health and Clinical Excellence thresholds for implementation.4


The extraordinary performance of this pilot confirms that taking lung cancer screening into communities using a lung health check approach is effective and can engage populations in deprived communities. The model of care required careful collaboration between primary care and commissioners, with the service delivered by and assured by a specialist cardiothoracic center. The success of the pilot has resulted in an expanded program to start in April 2019, with more than 10,000 lung health checks estimated. This is projected to result in more than 5,600 LDCT scans each year and approximately 175 lung cancer resections.
More recently, the National Health Service (NHS) has committed to rolling out the Manchester pilot across the United Kingdom in the NHS Long Term Plan 2019 (available in detail at longtermplan.nhs.uk). ✦
About the Author: Dr. Booton is programme director for the Manchester Lung Health Check Programme & clinical director for Thoracic Oncology at Manchester University NHS Trust, and honorary senior lecturer at the University of Manchester, United Kingdom.
References:
1. National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409.
2. Crosbie PA, Balata H, Evison M, et al. Implementing lung cancer screening: baseline results from a community-based ‘Lung Health Check’ pilot in deprived areas of Manchester. Thorax. 2018 Feb 13. [Epub ahead of print].
3. Crosbie PA, Balata H, Evison M, et al. Second Round Results from the Manchester ‘Lung Health Check’ Community-Based Targeted Lung Cancer Screening Pilot. Thorax. 2018 Nov 12. [Epub ahead of print].
4. Hinde S, Crilly T, Balata H, et al. The cost-effectiveness of the Manchester ‘lung health checks’, a community-based lung cancer low-dose CT screening pilot. Lung Cancer. 2018;126:119-124.











