By Sanja Dacic, MD, PhD, and Douglas J. Hartman, MD
Posted: December 2018
The pathology community initially showed resistance to digital pathology implementation in routine practice mostly because of pathologists’ lack of experience with the ever-changing technology, traditional thinking that review of digital images is more time consuming than light microscopy, and lack of approval from regulatory agencies. However, the U.S. Food and Drug Administration (FDA) approved the first whole-slide imaging system for primary diagnosis in April 2017. This decision should pave the way for standardization of digital pathology in practices and should encourage the pathology community to adopt digital diagnostic tools on a much larger scale.

Globalization of Pathology
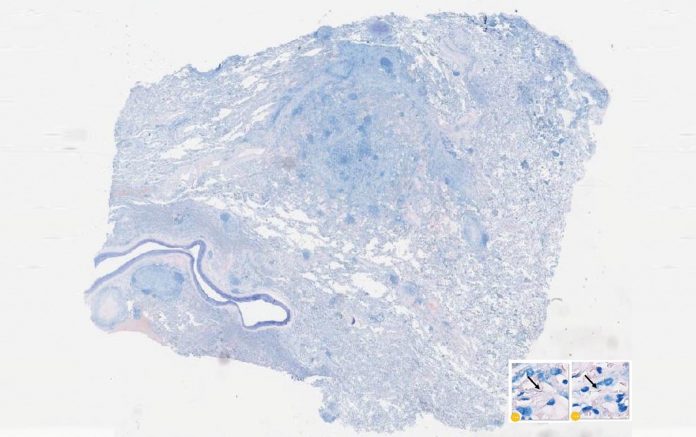
Digital pathology is a rapidly growing field that represents a significant part of pathology clinical practice in some medical centers, particularly in the areas of consultation, frozen section diagnosis, quality assurance quantification of immunohistochemical assays (i.e., PD-L1 and immune cells), and identification of microorganisms in tissue sections. The major advantage of digital pathology is the ability to create networks among pathologists, which allow them to efficiently share a large number of challenging cases either at the time of intraoperative consultation or for a second opinion. Pathology practices can also deliver services to remote locations without physical access to subspecialty expertise, which is particularly important given the increasing emphasis in the field on improving diagnostic excellence and quality. At the same time, providers, particularly in large academic centers, have the ability to archive noteworthy cases for teaching and research purposes, while enhancing revenues for their expanding consultation practices.

On the other hand, there is concern that the implementation of digital pathology may result in outsourcing of small pathology practices to centers with highly sought expertise, subsequently eliminating onsite pathologists in small hospitals or even across the world and leading to the globalization of pathology practice. This is a valid concern that has been already experienced with the development of the large integrated healthcare networks, although one has to keep in mind that high operating cost for implementation and maintenance of equipment needed for digital pathology services, together with identification of a team of skilled people who will make this service happen, might be challenging.
Although storage costs are decreasing, digital pathology still generates a large amount of data (200 MB to one-half GB per digital slide) and, therefore, cloud storage represents an attractive solution regarding equipment costs. Cloud-based services make images easily and, usually, more affordably accessible; however, these services can be vulnerable to external breaches (i.e., hacking). Therefore, data safety is a critical issue that hospitals must address. One recent improvement has been the development of a single repository to hold all imaging data for a healthcare network (i.e., enterprise imaging).
Emerging Complementary Technologies
Several nontraditional methods for examining tissue are being developed. These include super resolution, multiplex fluorescence, microscopy with ultraviolet sectioning excitation (MUSE), and optical coherence tomography/in vivo microscopy. In addition to these nontraditional methods, there have been technologic advancements with whole-slide imaging that cannot be achieved by light microscopy, such as 3D imaging. In the research arena, 3D reconstruction of whole-slide images has been used for classification of lung adenocarcinoma. This technology is not currently used in clinical surgical pathology, but it has made its way into forensic pathology as virtual autopsy (virtopsy). A current practice in pathology laboratories is to take static digital images of surgically resected specimens. Using 3D reconstruction technology, this could result in better radiologic–pathologic correlation as well as in improvements in radiologic interpretation. This approach may also improve the accuracy of the tumor-size measurement, which is a major determinant in the T staging of lung cancer.
Finally, artificial intelligence (AI)— deep learning, in particular—has been proposed as another tool that can improve and transform clinical practice. There is great enthusiasm for AI applications in radiology and cardiology imaging (e.g., MRI and ultrasound) that can potentially be automated to the point of generating a diagnosis. For radiology applications, AI has been mostly applied in a “second-look” function, so it seems reasonable that this functionality will also transition to digital pathology. It is difficult to predict where AI will be applied in pathology, but it will not replace pathologists in the near future because humans plus AI have performed better than each individually.1

In summary, the digital pathology space is starting to expand, having been given FDA approval. Digital pathology represents a disruptive technology that will facilitate more advanced diagnostic skills for pathologists. It should be viewed as another sophisticated tool in a pathologist’s armamentarium that can improve diagnostic accuracy and, subsequently, enhance the management of complex diseases by a multidisciplinary team, with the end result hopefully being better patient outcomes.
About the Authors: Dr. Dacic is a professor of pathology, University of Pittsburgh Medical Center, and is a member of the IASLC’s Pathology Committee. Dr. Hartman is an associate professor of pathology and associate director, Division of Pathology Informatics, University of Pittsburgh Medical Center. ✦
Reference:
1. Dreyer KJ, Geis JR. When machines think: radiology’s next frontier. Radiology. 2017;285(3):713- 718.










