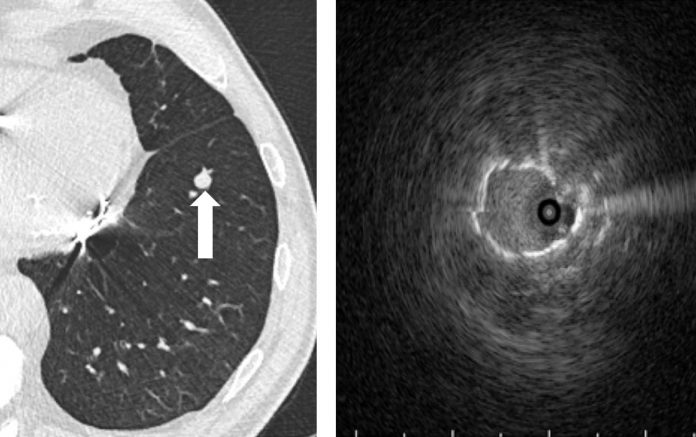
Bronchoscopy was undertaken with radial EBUS (right) to identify the lesion (Note that scale for the EBUS). Transbronchial biopsy demonstrated adenocarcinoma, and the patient received a left-lower lobectomy, with confirmation of a stage IA lung adenocarcinoma.
By Andrew R. Haas, MD, PhD
Posted: October 2018
Lung cancer remains the leading global cause of cancer-related mortality.1 Due to the lack of symptoms at the time early-stage disease first manifests, the majority of patients still present with advanced-stage disease.
Optimal treatment and patient outcome is incumbent on thorough radiographic and invasive staging. In addition, the rapid acceleration in development and use of targeted and immunotherapeutic agents as treatment options has obligated proceduralists to not only obtain a diagnosis and to ascertain nodal staging, but also to ensure adequate tissue acquisition to perform molecular and immunoprofi ling analyses. The development of advanced bronchoscopic diagnostic technology in the past decade has enhanced the capacity for pulmonologists to biopsy primary lesions, provide minimally invasive nodal staging, and obtain adequate tissue for tumor profiling from small-volume tissue samples.

Since the flexible bronchoscope was developed in 1966, there has been no greater technologic advance in diagnostic bronchoscopy than the introduction of curvilinear and radial endobronchial ultrasound (EBUS). More than a decade of clinical trials has demonstrated that lymph node staging by EBUS is not only effective and safe, but it can supplant mediastinoscopy for nodal staging when performed correctly and thoroughly.
With this mounting evidence in support of EBUS as an effective nodal staging modality, the third edition of the American College of Chest Physicians lung cancer guidelines added EBUS as the preferred method of initial lymph node staging in patients with suspected lung cancer and nodal involvement.2 EBUS nodal staging should follow a standard systematic approach via EBUS visualization from N3 to N1 nodal stations; any lymph node with a short axis greater than 5 mm should be sampled.
However, with the expanding portfolio of targeted and immunotherapeutic agents available for patients with unresectable malignancy, diagnostic and staging information alone from EBUS is no longer adequate. Additional material must be acquired to perform tumor molecular and immunoprofiling, and multiple studies have shown that biopsies obtained via EBUS needle aspiration, if sufficiently cellular, can be adequate to perform standard histologic, immunohistochemical, and molecular and immunoprofiling analyses.
Rapid on-site evaluation (ROSE) is used at many centers to identify malignancy, and often, further nodal sampling is ceased once a tumor is detected. This practice should be reconsidered for two reasons: the eighth edition of the IASLC lung cancer staging guidelines3 breaks the nodal status into subcategories of single-versus multiple-station disease; and tissue acquisition from more than one potentially involved site may improve the probability of having adequate material for all necessary tumor analyses. Repeat sampling of different areas within an involved node should also be considered to provide better material for analyses, especially if radiography or EBUS suggests the nodes are necrotic. An interesting ROSE application may be to semi-quantitatively assess the degree of sample cellularity to guide decisions regarding sample adequacy for all tissue analyses.
Navigation Platforms
Suspected peripheral lung cancers continue to pose challenges and limitations, but the development of radial EBUS and navigation platforms has improved the ability to approach some peripheral lesions for biopsy where access has been difficult. Navigation systems are based on two main platforms: electromagnetic (EMN) or virtual bronchoscopy.
Although single-center series of diagnostic yield using navigational platforms has reported diagnostic rates as high as 80% to 90%, only one randomized control trial has been performed comparing EMN to radial EBUS to EMN and EBUS combined. This study showed nearly equivalent diagnostic yield for EMN and radial EBUS alone (59% vs. 69%, respectively), but combined EMN and EBUS had a diagnostic yield of 88%.4 Therefore, in the absence of lesion selection bias, combined use of EMN and radial EBUS appears most effective to access and biopsy peripheral lesions. No study has been performed comparing EMN to virtual bronchoscopy.
The limitation of navigational bronchoscopy and radial EBUS is the reliance on airway access for lesion localization and biopsy. If no airway is adjacent to or within a lesion, existing navigational platforms and radial EBUS cannot adequately access a lesion for biopsy. Multiple approaches are under early investigation to provide an “out of airway” transparenchymal approach to those nodules to improve diagnostic yield. Efficacy and safety of these approaches will be forthcoming.
All patients should undergo thorough and complete EBUS nodal staging with consideration of either ROSE assessment of sample cellularity or acquisition of extra aspirations to maximize tissue available for analyses.
Real-World Decisions
How are bronchoscopists to use the new technologies at their disposal for the diagnosis, staging, and tumor profiling of lung cancer, particularly advanced-stage disease? All patients should undergo thorough and complete EBUS nodal staging with consideration of either ROSE assessment of sample cellularity or acquisition of extra aspirations to maximize tissue available for analyses. If the primary parenchymal lesion is easily accessible to transbronchial biopsy, consideration should be given to biopsy this lesion to maximize tissue for analysis, particularly PD-L1 immunohistochemistry, which is only validated on surgical pathology specimens. For suspected clinical stage 1A malignancy or suspicious solitary pulmonary nodules, advanced bronchoscopic techniques may not be the optimal first approach for a patient, and the respiratory physician must consider whether CT-guided needle aspiration or direct surgical resection would be a more prudent approach than using the latest bronchoscopic technologies.
What Is on the Horizon?
Bronchoscopic technology developments have all been inspired by the need to enhance minimally invasive diagnostic capabilities for nodal staging and peripheral nodule biopsy; however, bronchoscopists need to capitalize on the capacity of these technologies to deliver novel therapeutics directly to lymph nodes, masses, and/or nodules. Several bronchoscopic ablation devices for early-stage lung cancer are under development and in early-phase investigation. Investigations of these ablative devices must maintain clinical equipoise, as the safety and efficacy of stereotactic radiation creates a high standard to match. More importantly, with the expanding repertoire of targeted agents, viral and gene therapy vectors, adoptive cell therapies, and immunomodulating agents, respiratory physicians should work collaboratively with their thoracic oncology colleagues to design and to undertake novel trials of bronchoscopic-delivered therapies to further expand the armamentarium against lung cancer. ✦
About the Author: Dr. Haas is Associate Professor of Medicine, Director of the Interventional Pulmonary and Thoracic Oncology Program, and Bronchoscopy Director at the Hospital of the University of Pennsylvania.
References:
1. Cancer. www.who.int/en/news-room/fact-sheets/detail/cancer. Accessed February 12, 2018.
2. Silvestri GA, Gonzalez AV, Jantz MA, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2013;143(5 Suppl):e211S-50S.
3. Detterbeck FC, Boff a DJ, Kim AW, Tanoue LT. The Eighth Edition Lung Cancer Stage Classification. Chest. 2017;151(1):193-203.
4. Eberhardt R, Anantham D, Ernst A, Feller-Kopman D, Herth F. Multimodality bronchoscopic diagnosis of peripheral lung lesions: A randomized controlled trial. Am J Respir Crit Care Med. 2007;176(1):36-41.










