By Fabrice Barlesi, MD, PhD, and Eric Vallières, MD, FRCSC
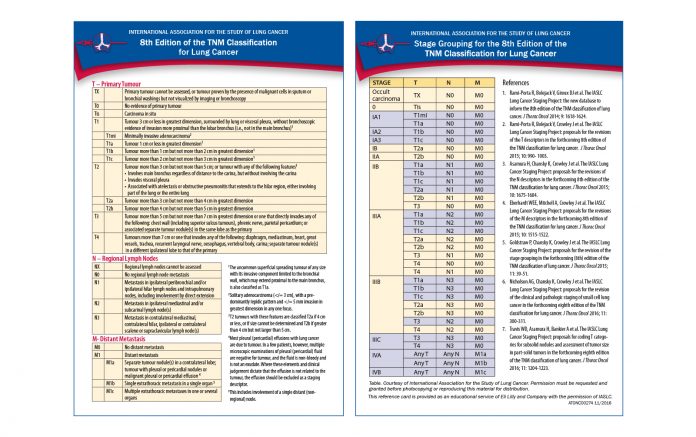
An article by Cynthia Kryder and Ramón Rami-Porta in the IASLC Lung Cancer News recently highlighted the innovations of the 8th Edition of the TNM Classification of Lung Cancer. This new classification is more detailed than the 7th edition, as it now contains 11 T descriptors, 6 N descriptors, and 4 M descriptors. These added “details” allow for a more precise prognostic assessment of the tumors, at the cost, however, of more complexity. This raises a crucial question. What are the potential practical consequences of this new classification?
In early stages, the prognostic value added by the centimetric division of the T components should have little impact on the local options for therapy whether one is dealing with surgery or radiosurgery per established treatment guidelines. The awaited results of randomized trials in Japan and North America addressing the role of lesser resections in tumors less than 2 cm in size could however potentially set new standards of surgical treatments for T1AN0 and T1BN0 tumors (stages 1A1 and 1A2). The 8th TNM classification also adds the categories of Tis and T1mi to differentiate the early adenocarcinomas with a lepidic component of AIS (adenocarcinoma in situ) and MIA (minimally invasive adenocarcinoma) from the more invasive adenocarcinomas of 3 cm or less in size: Tis tumors are now considered stage 0 and T1mi stage IA1. Finally, the new centimetric division at 4 cm (T2b) might be useful in more precisely determining the surgical population that may benefit from adjuvant chemotherapy after surgery (stages IIa and above as per the 8th edition) and therefore be helpful in designing and defining inclusion criteria for future adjuvant trials.
In locally advanced stages, and especially for patients with stage III NSCLC, introducing the concept of quantifying and describing the N status by the number of involved N1 and N2 stations (single versus multiple, N1 with N2, N2 without N1), although adding complexity, is a significant step in addressing the vastly different groups of node positive patients we treat. This delineation will help better define therapeutic strategies on or off trial for this very heterogeneous group of patients, where combined modality treatments are the norm. Indeed, the value of surgery, induction chemotherapy, and potentially adjuvant radiotherapy may be better characterized in the future on the basis of these new stage distinctions.
In advanced stages, the subclassification of the M component now separates patients with isolated extrathoracic metastasis (M1b) from those with multiple extrathoracic sites of disease (M1c), a differentiation that will be useful in an era where local consolidative therapy in selected cases of oligometastatic involvement has yielded strong PFS benefit in some clinical trials. It is anticipated that such strategies will be used more frequently in the future, especially in the case of oncogenic-addicted tumors.
As stated above, the 8th TNM classification, although more complex than previous iterations, has both practical and clinical research implications and consequences. Lung cancer clinicians will need to become familiar with this new TNM classification and to learn how to use it to its full potential. Hopefully, as in the past, the IASLC will be able to provide ample tutorial and educational material to its members and to the international lung cancer community to help with the transition. ✦
References
1. Gomez DR, Blumenschein GR Jr, Lee JJ, et al. Local consolidative therapy versus maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer without progression after first-line systemic therapy: A multicentre, randomised, controlled, phase 2 study. Lancet Oncol. 2016;17:1672-1682.