Posted: June 2017
By John K. Field, PhD, FRCPath and James L. Mulshine, MD, PhD
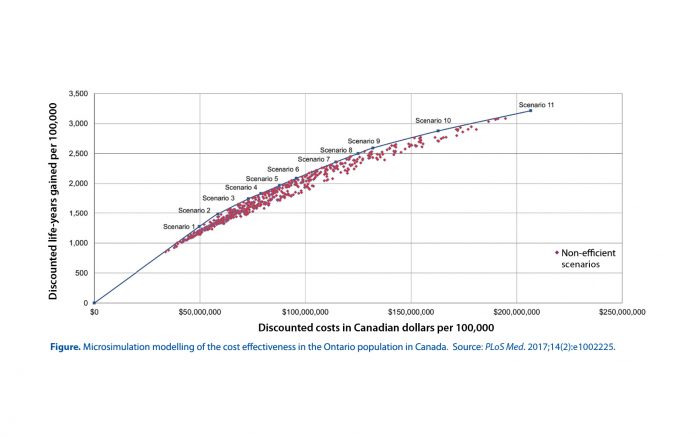
There is now robust and consistent evidence for the cost-effectiveness of lung cancer computed tomography (CT) screening as delineated in the recent analysis from ten Haaf and colleagues in PLOS Medicine.1 They have used microsimulation modeling analysis based on the smoking behavior surveys of individuals born between 1940 and 1969 from Ontario, Canada. Over 570 potential screening scenarios were evaluated, which included parameters such as the age to start or stop screening, screening interval, eligibility criteria (with respect to smoking history and quit time) as well as whether or not former smokers were excluded from further screening. Smoking criteria were based on both the National Lung Screening Trial (NLST) and the NELSON data. The costings were conducted from a third-party health care provider using Ontario Health Care plan. The results were provided as net discounted costs and life-years gained for each scenario. Their analyses are presented in the Figure below and demonstrate the results of all of the simulations of various screening scenarios on the efficient frontiers. The authors worked on $50K Canadian dollars (CD) per life-year gained, which is acceptable as the threshold for the Canadian health care system (i.e., US $41K and UK £28K). It is of note that these figures are significantly lower than the cost effectiveness figures from the NLST, (US $81K quality-adjusted life-year [QALY]), probably reflecting that the NLST did not have a standardized management process and the costly nature of the health care system in the US.2
Their results indicated that annual screening was more cost-effective than biennial screening and that scenarios that required higher levels of accumulated smoking exposure were more costeffective. They opined that the annual scenario of individuals 55-75 years old who smoked >40 pack-years and who currently smoked or quit <10 years ago has an ICR of CD $41K.1 An earlier lung cancer cost-effectiveness modeling study based on Canadian data, suggested CD $52K per QALY gained, which was improved by incorporating an adjunct smoking cessation program,3 which improved the quit rate by 22.5% and further improved the incremental costeffectiveness ratio to CD $24K per QALY.3
These results are consistent with the previously published actuarial approach by Pyenson et al,4,5 which estimated the costs and benefits of annual lung cancer screening on a commercial insurance model for the 50- to 64-year-old highrisk individuals. From Pyenson’s simulation, annual CT screening5 of individuals with 30+ pack-years (PKY) of smoking was associated with a QALY cost of US $28K. However, incorporating the provision of standard smoking cessation measures into the model modestly increased cost but resulted in an improvement in the QALY’s saved to somewhere between US $16K- US $23K.
Expressed another way, the cost of providing lung cancer screening as an insurance service in the US using an actuarial approach would be estimated at a cost of US $2.22 monthly per covered life compared to a calculated cost of US $1.02 in lung cancer screening if tobacco cessation services were included.6
Lung cancer cost-effectiveness has been mainly considered in the US context, which has a much more expensive health care system than that of Europe. The only cost-effectiveness data from a screening trial in Europe has come from the UK Lung Cancer Screening (UKLS), which was based on modeling using the baseline data, providing a figure of around UK £8.5K per QALY gained for screening.7
The modelling studies summarized above uniformly demonstrate that lung cancer CT screening is cost-effective. However, the major issue now is how best to implement lung cancer CT screening in different settings and how best to reduce the cost of delivering lung cancer screening in different international health care systems?
References
1. ten Haaf K, Tammemagi MC, Bondy SJ, et al. Performance and cost-effectiveness of computed tomography lung cancer screening scenarios in a population-based setting: A microsimulation modeling analysis in Ontario, Canada. PLoS Med. 2017;14(2):e1002225.
2. Black WC, Gareen IF, Soneji SS, et al. Costeffectiveness of CT screening in the National Lung Screening Trial. N Engl J Med. 2014;371(19):1793- 802.
3. Goffin JR, Flanagan WM, Miller AB, et al. Costeffectiveness of Lung Cancer Screening in Canada. JAMA Oncol. 2015;1(6):807-13.
4. Pyenson BS, Sander MS, Jiang Y, Kahn H, Mulshine JL. An actuarial analysis shows that offering lung cancer screening as an insurance benefit would save lives at relatively low cost. Health Aff (Millwood). 2012;31(4):770-9.
5. Villanti AC, Jiang Y, Abrams DB, Pyenson BS. A cost-utility analysis of lung cancer screening and the additional benefits of incorporating smoking cessation interventions. PLoS One. 2013;8(8):e71379.
6. Pyenson B, Dieguez G. 2016 reflections on the favorable cost-benefit of lung cancer screening. Ann Transl Med. 2016;4(8):155.
7. Field JK, Duffy SW, Baldwin DR, et al. The UK Lung Cancer Screening Trial: a pilot randomised controlled trial of low-dose computed tomography screening for the early detection of lung cancer. Health Technol Assess. 2016;20(40):1-146.