Posted: April 2017
By Cynthia L. Kryder, MS, CCC-Sp, with Ramón Rami-Porta, MD
Clinicians around the world began implementing the 8th edition of the tumor, node, and metastasis (TNM) classification of lung cancer on January 1, 2017. There has been confusion, however, over when the 8th edition of the TNM staging system will be fully implemented in the U.S. While the staging system has been implemented by the Union for International Cancer Control (UICC) as of January 1, 2017, the U.S. American Joint Committee on Cancer (AJCC) has delayed implementation until January 1, 2018. The reason for this is to ensure that that all partners in U.S. patient care and cancer data collection are working in synchrony, which the time until January 2018 will allow.
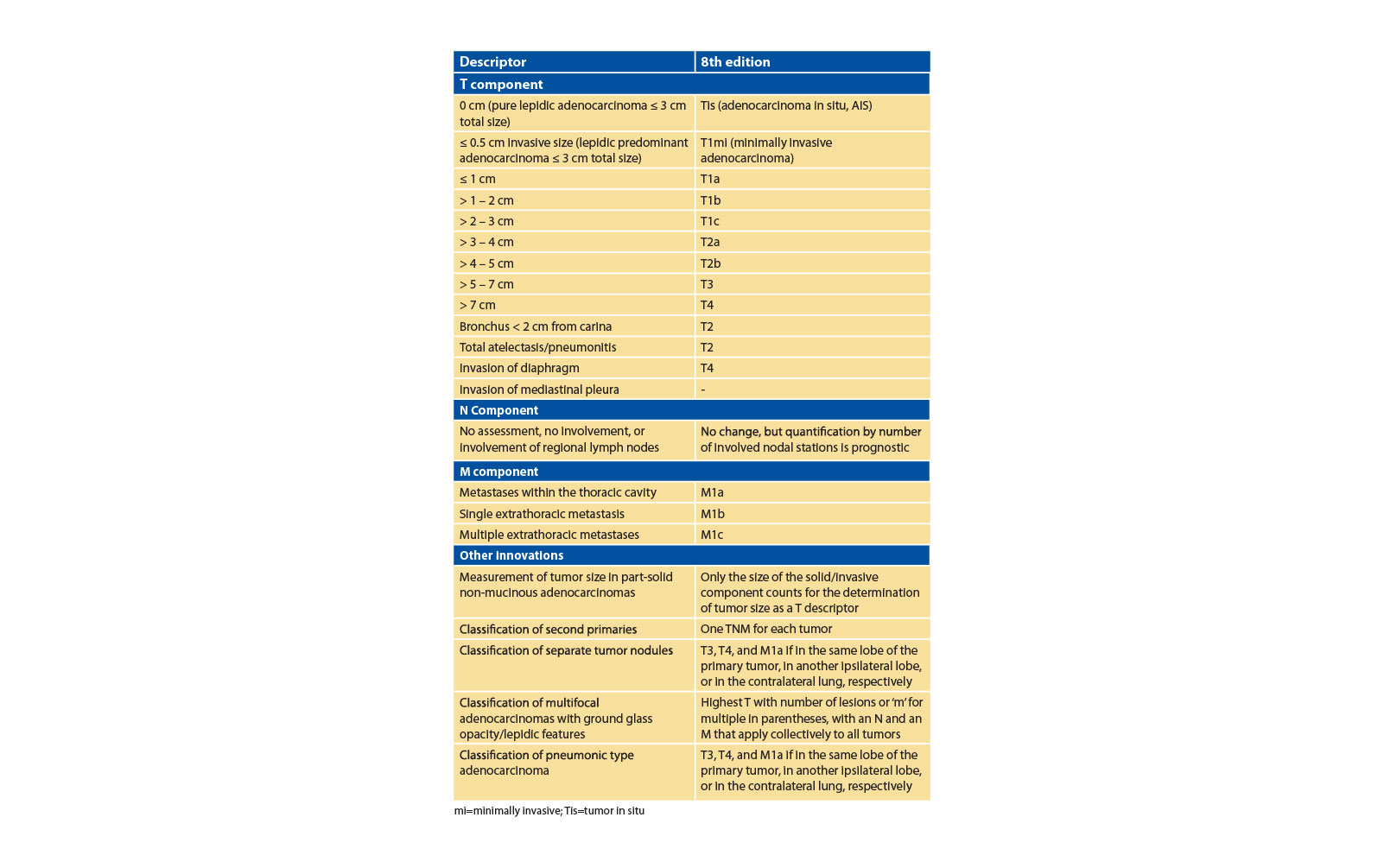
The revisions included in the TNM staging classification update represent a data-driven approach to the staging of lung cancer that features several innovations that will enhance prognostic capabilities and enable improved tumor stratification in future clinical trials. These innovations were informed by an analysis of data from the International Association for the Study of Lung Cancer (IASLC) database that included 70,967 evaluable patients with non-small cell lung cancer and 6,189 with small cell lung cancer. In particular, the 8th edition reflects an increased recognition of tumor size as a relevant prognostic factor as well as the prognostic significance of tumor burden in hilar and mediastinal lymph nodes and the prognostic impact of the number and anatomic location of metastatic tumors. The table summarizes the innovations introduced in the 8th edition of the TNM classification of lung cancer.
The T Component
Within the T component, new categories— adenocarcinoma in situ (Tis, AIS) and minimally invasive adenocarcinoma (T1mi)—were introduced based on tumor size and radiological and pathological features, endobronchial location < 2 cm from carina and total atelectasis/pneumonitis were downstaged from T3 to T2, and invasion of the diaphragm was upstaged from T3 to T4. In addition, visceral pleural invasion and its 2 categories (PL1: invasion beyond its elastic layer and PL2: invasion of the pleural surface) were confirmed as important prognostic factors.
The analyses of tumor size in the IASLC database provided evidence to support further subclassification of tumors 3 cm or less in size (T1 category in the 7th edition) and those greater than 3 cm (T2 category in the 7th edition), and to distribute tumor size as a descriptor of all T categories. Consequently, precise tumor size measurement is now more important than ever before, as small changes in size mean important changes in prognosis. Although the 3-cm cutoff point separating T1 and T2 tumors remains valid, survival analyses according to 1-cm cutoff points showed that from 1 to 5 cm, every centimeter counts. Larger tumors were associated with a worse prognosis than determined in previous TNM classifications and are better aligned with either T3 (tumor size of more than 5 to 7 cm) or T4 (tumor size of more than 7 cm).
The N Component
There are no changes in the N categories; however, the analyses for the 8th edition explored the quantification of nodal disease and found that the number of nodal stations involved had prognostic implications. The more nodal stations involved, the worse the prognosis. In addition, the prognosis of tumors with involvement of multiple N1 stations was similar to that of tumors with single station N2 without concomitant N1 disease (skip metastases).
Nodal quantification is classified as:
• N1a: involvement of a single N1 nodal station
• N1b: involvement of multiple N1 nodal stations
• N2a1: involvement of a single N2 nodal station without N1 involvement (skip metastasis) • N2a2: involvement of a single N2 nodal station with N1 involvement
• N2b: involvement of multiple N2 nodal stations
The M Component
Refinements to the M component include different categories for single and multiple extrathoracic metastases in one or in several organs. There is no change in the designation of metastasis within the thoracic cavity (M1a); however, since single extrathoracic metastases have better prognoses than multiple extrathoracic metastases in one or in several organs, different categories have been defined for them: M1b for single and M1c for multiple extrathoracic metastases. Prognosis is similar for M1a and M1b tumors. Nevertheless, they represent distinct forms of metastatic involvement that require different approaches to diagnosis and treatment, justifying the need to define them separately.
Stage Grouping
Some TNM subsets have moved from one stage to another, and new stages and substages have been created to accommodate groups of tumors with similar prognoses. Taxonomic changes, however, do not necessarily dictate an automatic change in therapy if the clinical trials performed to test therapeutic options did not originally include the tumors that are now included in the selected stages for study. In the absence of results from clinical trials, clinical judgment will determine the best therapeutic options for a given patient with a given tumor.
Clinicians should be aware of the following stage changes:
• Stage IA is now divided into stages IA1, IA2, and IA3 to include the new T1a, T1b, and T1c N0M0 tumors
• Stages IB and IIA now denote T2aN0M0 and T2bN0M0 tumors, respectively
• All N1M0 tumors are now stage IIB, together with T3N0M0 with one exception: T3-T4N1M0 tumors are now stage IIIA
• All N2M0 tumors are now stage IIIA, except for T3-T4N2M0 tumors, which are in stage IIIB, together with all N3M0 tumors, except for T3-T4N3M0 tumors, for which a new stage IIIC was created
• Stage IV is now divided into stage IVA to group M1a and M1b tumors and stage IVB to include M1c tumors
In summary, the 8th edition of the TNM classification of lung cancer introduces new groups based on tumor size, validates the prognostic importance of quantifying nodal disease, establishes a new category for single extrathoracic metastasis, and defines new stage groupings that more closely align with expected prognosis. These refinements enable a better understanding of the anatomic extent of the tumor and help clinicians refine both a clinical and pathologic staging. In so doing, these changes will require greater attention in measuring tumor size, determining nodal disease status, searching for metastases, and using clinical judgment to determine treatment. ✦











