Posted: April 2017
By Anne Fraser, Oncology Nurse Practitioner
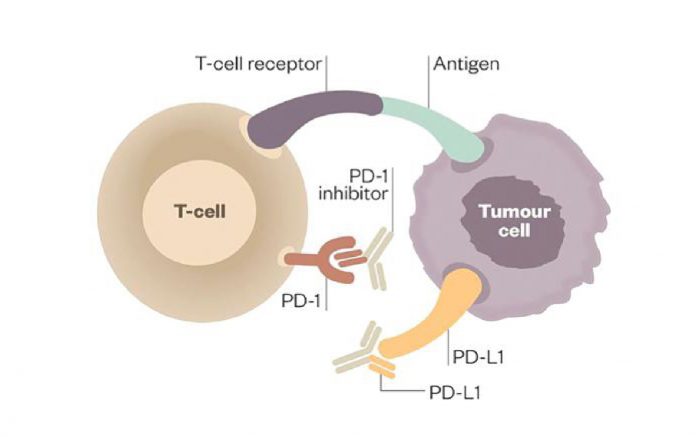
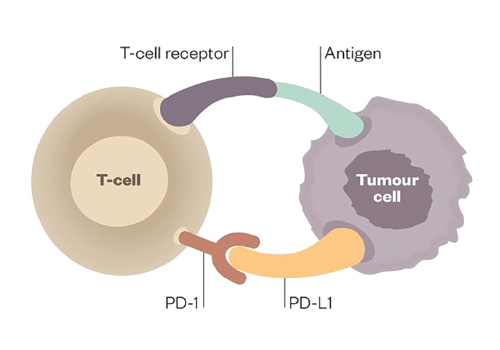
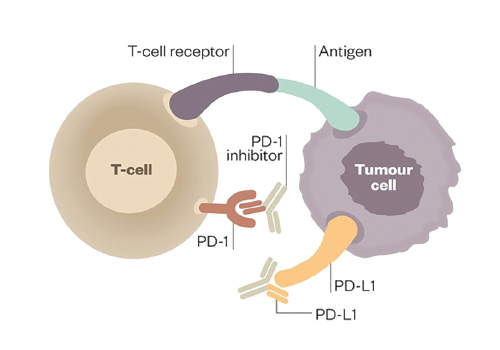
Immunotherapy has changed the landscape of lung cancer treatment, offering hope to advanced lung cancer patients. Immunotherapy works by activating the patient’s immune system, helping it to better fight and destroy the cancer cells. Cancer cells evade death from T cells by expressing PD-L1 (programmed death ligand 1), which then deactivates the T cell by binding to PD-1 on the surface of the T cell. Immunotherapies target PD-1 or PD-L1, preventing the tumor from suppressing T cells and allowing the T cells to kill the cancer cells (Figures 1 and 2).
Treatment with immunotherapies is not without risks, and patients may experience a wide range of side effects, including serious adverse events. Common patientreported events include rash, fatigue, pruritus, diarrhea, arthralgia, nausea, vitiligo, asthenia, myalgia, headache, fever, decreased appetite, and cough. More serious immune-mediated adverse events include pneumonitis, endocrinopathies including hypothyroidism and hypophysitis, colitis, hepatitis, and nephritis. The key to managing such side effects of treatment is early recognition and close communication with the patient. Nurses and allied health staff play a key role in early intervention. Patients may require a break from therapy for many months and the use of high-dose steroids to manage Grade 2 or higher toxicities. In these situations, patients require close monitoring and support. Grading of toxicities should be done in conjunction with the NCI-CTCAE guidelines; the latest version can be found on this link: http://evs.nci. nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_8.5×11.pdf
At the recent IASLC 17th World Conference on Lung Cancer, held in Vienna December 4-7, 2016, the Nurses and Allied Health (N&AH) Committee were kindly sponsored by IASLC to attend a workshop with the aim of developing clinical guidelines for the management of patients receiving immunotherapies (Figure 3). The group consisted of nurses from Australia, New Zealand, the United States, the United Kingdom, Hong Kong, and Denmark. Each regional group had completed work on clinical management prior to arriving in Vienna, and this was presented to the wider group for further discussion and consultation. There were lively debates as regional management proved to vary in some cases. One of the aims was to produce a guideline that would be useful in all clinical settings—for those countries with limited clinical resources and for those clinicians who do not have the support of a wider oncology team. This led to thoughtful discussion about clinical resourcing for lung cancer patients worldwide, with a particular focus on the lack of skilled nurses and the lack of utilization of allied health staff in the clinical setting. The N&AH Committee of IASLC intends to publish and disseminate these guidelines in 2017. ✦