Posted: February 2017
By Lori Alexander, MTPW, ELS, MWC
WCLC 2016 offered focused education for nurses and allied health professionals through its nursing track, as well as through special nursing workshops held before the official start of the conference. The sessions addressed a range of topics, including the use of technology and social media, preparing patients for treatment, managing toxicities of newer treatments, and smoking cessation.
The International Thoracic Oncology Nursing Forum (ITONF) presented “Innovating Lung Cancer and Mesothelioma Care,” an extensive educational workshop that covered such topics as immunotherapy, clinical trials, vaping and smoking cessation, and social media and e-health. One highlight of the workshop was “Leveraging Technology and Social Media in Nursing,” presented by Anne Ireland, MSN, RN, AOCN, CENP, City of Hope National Medical Center, Duarte, US. Ms. Ireland discussed specific technologies that will provide opportunities for better data collection and integration, including wearable health-tracking devices, video capabilities, and real-time communication.
“Health and fitness apps have created an entirely new way of communication between providers and patients, making remote monitoring and health promotion easier and more cost-effective,” Ireland said. “The opportunity to use apps for health promotion and monitoring seems endless and provides for ease of access not previously possible.”
Such technology was also a topic at “Supporting Patients Receiving Treatment,” where Roma Maguire, Professor of eHealth, University of Surrey, Guildford, UK, discussed the use of mobile phone technology to remotely monitor patients. Ms. Maguire described mobile systems for patient-reported outcome measures; these systems enable systematic assessment, real-time recording of symptoms, and rapid therapeutic response. Another technologic tool, an electronic symptom management system, guides patients through a series of questions about their symptoms and then provides automated evidence-based self-care advice in response to the answers. Both tools facilitate patient-centered care and give patients access to care regardless of their geographic location.
Thoracic oncology nurses face very different challenges depending on the treatment being administered to their patients, and the side effect profiles of tyrosine kinase inhibitors (TKIs) and immunotherapy differ substantially from those of chemotherapy drugs. Although nurses now have more than 10 years of experience with TKIs, toxicities can still be very difficult to grade and manage.
Beth Eaby-Sandy, CRNP, University of Pennsylvania, Philadelphia, US, discussed rashes and other cutaneous toxicities associated with EGFR inhibitors, including paronychia, hypertrichosis, trichomegaly, fissuring, pruritis, and xerosis. Rashes associated with EGFR inhibitors can be severe and can affect patients’ quality of life, have an impact on activities of daily living, and even cause dose reductions. Despite the challenges, it is imperative for nurses to manage rashes and keep patients on therapy, said Ms. Eaby-Sandy, because of a correlation between the side effect and overall survival.
“Identification, prevention, and management are important tasks for oncology nurses to master to allow patients to remain on therapy,” she said. Ms. Eaby- Sandy added that it is important to tailor management strategies to a patient’s symptoms, side effects, specific drug, and dosage.
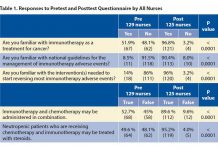
In contrast to TKIs, immunotherapy appears to have limited toxicity. However, immunotherapy presents unique nursing challenges, said Rachel Thomas, lung cancer clinical nurse specialist at Guy’s and St. Thomas’ National Health Service (NHS) Trust, UK. She noted that, although clinical trial data demonstrate that patients receiving immunotherapy have better overall survival and outcomes, she has seen a mixed response to treatment.
“There have been many stories in the newspapers which report that immunooncology drugs are a miracle treatment for patients with lung cancer. This can often give patients false hope and can lead to distress when they find they are not eligible for the treatment or when the treatment is not effective,” Ms. Thomas said. “Part of our role is to ensure patients are well informed but have reasonable expectations of the outcomes of treatments.”
“Nurses continue to be underutilized in global tobacco control efforts,” said Stella Bialous, RN, DrPH, University of California, San Francisco, School of Nursing, US, who spoke at the nursing session “Prevention.” She urged nurses and other allied health professionals in all settings—primary care clinics, hospital wards, palliative care settings, and everywhere in between—to intervene with evidence- based smoking-cessation practices during all stages of the cancer continuum, not only as a measure of cancer prevention but also from screening to treatment and through survivorship.
“When properly educated, [nurses] can make a significant difference in reducing the suffering from tobaccorelated diseases,” said Ms. Bialous.
Speaking at the same session, Iveta Nohovova, MA, Charles University Prague, Czech Republic, also discussed the role of oncology nurses in smoking cessation. Ms. Nohovova said that nurses, as the largest health care group, have a moral obligation to be smoke-free role models for their patients, their families, and society as a whole. She added that nurses should not underestimate the unspoken influence they carry.
Content from the ITONF workshop is available on its website (http://itonf.com/), and slides from the WCLC 2016 nursing sessions are available in the IASLC Virtual Library (http:// library.iaslc.org/). IASLC Lung Cancer News will continue its focus on the role of nurses in the care of patients with lung cancer in subsequent issues, with forthcoming articles on the toxicities of immunotherapies and the challenges of implementing the advanced practice nursing role globally, among other topics.