By Sanjay Popat, FRCP, PhD
United Kingdom Healthcare System
The United Kingdom (UK) has a unique healthcare system: the National Health Service (NHS), a publicly funded, singlepayer system. Founded by the Labour government in 1948, its unique identity is constitutionally defined as a comprehensive service delivered to all, based on clinical need and not on ability to pay, and funded by general taxation. In practice, this means that healthcare is free at point of use for most services, including cancer treatment.1 So, if cancer care is free in the UK, who decides which treatments are funded (reimbursed) and which ones aren’t? The answer is surprisingly complex, geographically different, and very much depends on treatment type; for example, cancer surgery is funded differently from new anti-cancer drugs. The key organization to manage cancer commissioning, though, is the National Institute for Health and Care Excellence (NICE). This is a non-departmental public body established by primary legislation, accountable to the UK Department of Health, but operationally independent of it, with a remit only technically for England, but with arrangements in place for the devolved nations (Wales, Scotland, and Northern Ireland).2
What Does NICE Do?
As the NHS is funded through general taxation, with a fixed budget allocated to the Department of Health from the government, some entity therefore needs to decide if new drugs should be funded, and if so, on what grounds: enter NICE. NICE is extremely active. It provides evidence-based guidelines, information services for commissioners and clinicians, and defines quality standards and performance metrics. However, perhaps the most important oncological role of NICE is providing funding approvals. In this regard, NICE issues decrees on the cost-effectiveness of new “technologies” (e.g., a new anti-cancer drug, medical device, diagnostic test) to the NHS.
How Does NICE Appraise New Drugs?
The process by which NICE appraises new drugs has changed recently, but the principles remain similar. Previously, NICE would only appraise a new indication after EMA licensing, a process that often took over a year to complete in practice. Given that EMA licensing often took many months after presentation of phase 3 trial data, the net effect was that patients were potentially denied access to effective anti-cancer therapy, frequently for over 1 year, assuming that NICE eventually recommended funding. Reacting to this, the government initially established the Cancer Drugs Fund (CDF) and ultimately reformed NICE processes.
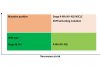
So how exactly does NICE determine cost-effectiveness? This is the critical issue. NICE determines the most likely cost per quality-adjusted life-year (QUALY) by principally receiving evidence from the manufacturer and a commissioned independent academic “evidence review group.” The QUALY threshold is not fixed by NICE but from analyses of historical outcomes; this seems to be around £40K per QUALY.3 This assessment method may be problematic for modern therapeutics since considerable uncertainties in determining the true QUALY often exist, particularly when the magnitude of the survival benefit afforded is unknown and or needs estimation (e.g., TKIs where patients crossed over, either per trial or in routine care, or for single-arm phase 2 data). In addition, the manufacturer’s base cost of most drug indications submitted usually prices nearly all indications beyond NICE’s historical approvals thresholds. As a result, either indications are rejected/decommissioned by NICE (e.g., erlotinib in the BR.21 indication), or substantial delays ensue prior to ultimate approval by NICE while manufacturers negotiate confidential discounted NHS pricing, or manufacturers simply decide not to submit appraisals (e.g., bevacizumab or alectinib).
What’s the Solution?
NICE undoubtedly performs an essential function by rationing a fixed budget, driving down the cost of new medicines for the NHS, and by allowing confidential discounts from manufacturers. Several improvements to the NICE process have been made recently; NICE now reviews potential indications parallel to licensing with three potential outcomes: the drug is approved for funding, rejected, or recommended for a limited period in a new Cancer Drugs Fund (if there is uncertainty for cost-effectiveness) pending reappraisal. Additionally, a new Early Access to Medicines Scheme (EAMS) has been developed, allowing prelicensing access to promising innovative medicines. All of these changes are deeply welcome. Nevertheless, the fundamental issues of eye-watering drug base costs and NICE cost-effectiveness methodology remain unchanged. While progress has been made, it is clear that the dance between NICE and manufacturers leaves patients and clinicians in a difficult position. “It takes two to tango” is a common English idiom. Let’s hope that the dance is over quickly! ✦
References
1. https://www.gov.uk/government/publications/the-nhs-constitution-for-england. Accessed September 23, 2016.
2. https://www.nice.org.uk/about/what-we-do. Accessed September 23, 2016.
3. Dakin H, Devlin N, Feng Y, Rice N, O’Neill P, Parkin D. The Influence of Cost-Effectiveness and Other Factors on NICE Decisions (2015): 24;10: 1256–1271.