By Cynthia L. Kryder, MS
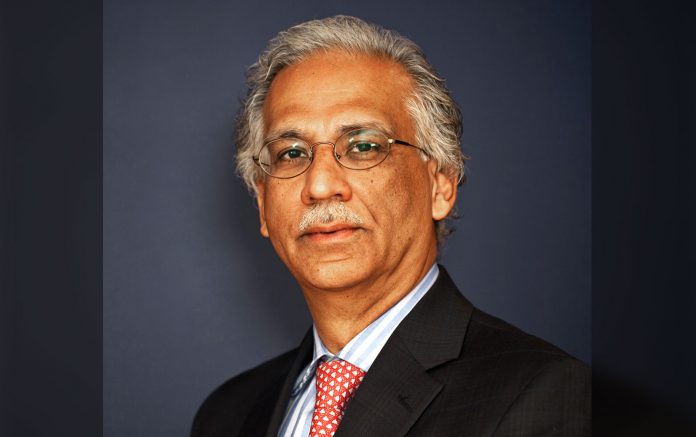
IASLC Lung Cancer News recently spoke with Kapil Dhingra, MD, of KAPital Consulting LLC in Sparta, New Jersey, about oncologic drug development and the challenges and opportunities to anticipate in the future.
Q: What are the perils and pitfalls of oncologic drug development in the new millennium?
A: I don’t necessarily agree with the phrase “perils and pitfalls.” From my perspective, we are experiencing the golden age of oncologic drug development with a plethora of targeted drugs and immunotherapies at our disposal and even more in development. This is an exciting time and we need to maintain this momentum to harness the power of personalized medicine in the treatment of cancer.
That said, we are facing several challenges. We still have a relatively poor understanding of what makes cancer cancer and what makes cancer respond or not respond to treatments. The connection between the tumor cell, its microenvironment, and the immune system is complicated and the tools available to understand complex cancer biology remain poor. For instance, we have no way of knowing what goes on in a patient’s tumor once we’ve administered a drug.
Another big challenge is the competitive oncologic drug-development environment. There is tremendous pressure from all stakeholders on small and large companies to bring first-in-class drugs to market quickly. This competition often leads to suboptimal decision-making. Judicious acceleration of drug development while maintaining an objective perspective on the emerging early data on new drugs is critical to achieve the right balance.
Q: How do we address the risk-benefit equation in the development of targeted therapies and immunotherapies?
A: Nothing has really changed in a meaningful way as to how we assess risk versus benefit, whether we’re talking about chemotherapy, targeted therapies, or immunotherapies. With any drug, we still need to weigh its benefit against the price to be paid with regard to side effects. Our hope is that targeted therapies and immunotherapies will yield a better risk: benefit profile compared with chemotherapy. The key change is in our expectation that we are no longer interested in drugs that produce modest improvements in survival at the expense of significant toxicity.
Q: Is lung cancer unique in this regard?
A: No.
Q: Given the stakes in cancer therapy and the imminent lethality of cancer, shouldn’t some of the rigid rules developed by the FDA in the management of “benign” illnesses like hypertension or diabetes mellitus be relaxed?
A: In my opinion, the FDA has become much more enlightened over the past 5 or 6 years. The FDA has shown significant flexibility with oncologic drug trials by allowing sponsors to combine phase 1, 2, and 3 trials into one trial. Similarly, the FDA has been open to considering new ways to assess the efficacy of targeted therapies and immunotherapies. Keep in mind that the vast majority of novel oncology agents are approved not based on their effect on overall survival, but on other endpoints such as disease-free survival and progression-free survival. Even in the European Union, regulators have shown considerable flexibility in approving new targeted cancer drugs. This represents a change from the way drugs were approved in the past. In addition, mechanisms to accelerate the speed of approval of cancer drugs have been implemented. Consequently, in the last 5 years, more than 40 new agents to treat cancer have been approved. So, from that perspective, the FDA already has relaxed its traditional regulatory framework.
Q: We seem to obsess about QT intervals. Millions of dollars have been expended in drug development focusing on serial electrocardiograms (ECGs) in cancer treatment studies. Is this money well spent? Don’t nearly all agents cause QTc prolongation? Are there other, more relevant, toxicities we should focus on?
A: I don’t see this as a big issue. Certainly QTc prolongation is more relevant outside of oncology. The oncology drug development community became more aware of it as a number of tyrosine kinase inhibitors moved through clinical development. But, to my knowledge, the FDA has never used QTc prolongation as the sole or even a primary reason to reject an oncology drug for approval if the drug otherwise provided a meaningful benefit. The sponsors can negotiate with the FDA as to when a dedicated QTc clinical study should be done during the development plan.
We do need to shift our focus, though, with regard to toxicities when using these novel agents. It was perfectly acceptable to focus on grade 3 and 4 toxicities such as reversible myelosuppression when dealing with chemotherapeutic agents. But when we’re dealing with targeted therapies and immunotherapies that are given long term, we need to look at persistent grade 1 and 2 toxicities. A grade 2 skin rash or diarrhea that persists over a long period of time can adversely affect a patient’s quality of life far more than grade 3 myelosuppression, which is often asymptomatic. Also, with immunooncology drugs, we are seeing far more toxicities, e.g., autoimmunity, that linger long after a drug is stopped.
Q: If an effective drug in class exists, should the rules change for subsequent drugs in the same class?
A: Yes. Given the imminent risk to the patient, it is often unethical to deny or stop a drug that is working for a patient. This is quite different than other “benign” chronic diseases where placebo-controlled (often meaning no active treatment) trials are eminently feasible. This does not necessarily mean that a new drug should per se be held to a higher standard than another drug in the same class. However, there should be reasonable assurance that a new drug is not inferior to an already approved drug in the same class.
Q: Is there anything else you would like to share with our readers about oncologic drug development in the future?
A: The lung cancer drug development community needs to develop a more holistic approach to profile the patients’ tumors. This should include not just actionable mutations such as EGFR mutations and ALK fusions, but also the microenvironment and the homeostasis between the tumor and the patient’s immune system. Additionally, we need to develop more systematic and efficient means to test the large number of permutations and combinations of novel agents in the pipeline. Serial profiling of the tumor and the patient’s immune system will enable us to offer a more personalized approach to treatment of the majority of patients with lung cancer, rather than a minority of patients who qualify for such an approach today. I foresee a future where such profiling will be done not only at baseline, but also several times during the natural history of a patient to adapt his/her treatment regimen or regimens to the emerging changes in the behavior of the tumor.
There have been major advances in our understanding of tumor biology including genetic changes, the role of the tumor microenvironment and factors regulating the immune system. These advances have impacted our clinical development paradigms with an increased focus on precision medicine based on tumor genetic changes and a characterization of the immune status of the tumor. This should result in improved selection of patients for therapeutic regimens, especially the development of novel combination therapies. As oncology clinical development has evolved in terms of trial design and endpoints, there have also been regulatory changes such as the FDA Breakthrough Therapy Designation. This evolution has resulted in additional productive discussions between sponsors and regulators to speed the approval of therapies for unmet medical need. In summary, as Dr. Dhingra states, we are in an exciting era of drug development and the pace of advance should provide important new therapies to cancer patients.
— Richard B. Gaynor, MD Sr. Vice President, Oncology Business Unit at Eli Lilly and Company