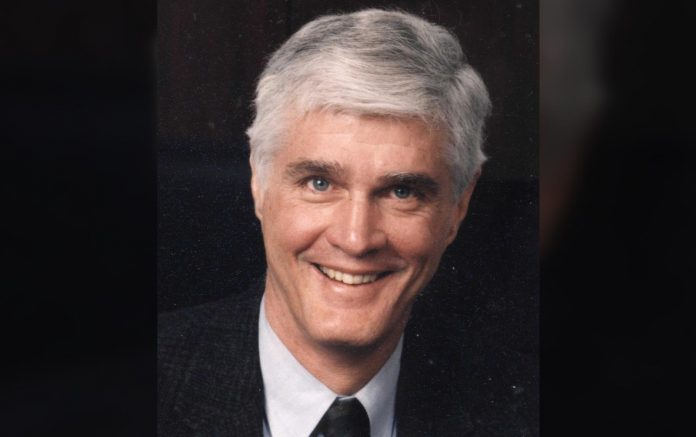
The David A. Karnofsky Memorial Award from the American Society of Clinical Oncology (ASCO) recognizes oncologists who have made outstanding contributions to the research, diagnosis, or treatment of cancer. Dr. Paul A. Bunn, Jr, Distinguished Professor, Division of Medical Oncology/ University of Colorado, James Dudley Chair in Lung Cancer Research, is the 2016 Karnofsky Award recipient and was interviewed by IASLC Lung Cancer News. The following “perspective” constitutes an abridged summary of Dr. Bunn’s reflections and comments:
Although the Karnofsky Award is given to individuals, cancer research is an inherently collaborative endeavor, one in which current progress is possible only due to the efforts of those who came before. Historically, representatives from the field of thoracic cancer research have been underrepresented as recipients of this award, and my selection can be seen as a recognition that the sustained efforts of many individuals has led to important recent advances in lung cancer.
Efforts by members of the International Association for the Study of Lung Cancer Pathology and Staging Committees to improve the systematic pathology classification and the TNM IASLC staging of lung cancers have helped clinicians to choose the best treatments for each individual patient. Spiral computed tomography (CT) scans have reduced mortality by improving early detection, and the push by IASLC, government, and non-government agencies to reduce smoking rates has made a huge impact on reducing the incidence of lung cancer. Advances in radiation and surgery have improved cure rates with decreased mortality and morbidity. Molecular therapies, targeted therapies, and immunotherapies have helped improve the outcomes for advanced patients considerably. Obviously, I am not responsible for all of these advances, and so I view this award as a tribute to all who have contributed to advances in prevention, early detection, pathology, staging, and treatment of lung cancer.

The history of systemic cancer treatments began after the end of World War II with the discovery that nitrogen mustard could be used to treat leukemias and lymphomas. In the 1950s, Sidney Farber showed that antifolates like methotrexate could be used to treat acute lymphoblastic leukemia. Subsequently, Drs. Emil “Tom” Frei III and Emil J. Freireich and others tested combinations of chemotherapeutic agents to try to cure leukemia, and Dr. Vincent DeVita and colleagues showed that combination chemotherapy could cure Hodgkin disease and other lymphomas. Despite these improvements, however, the field of oncology lacked a biological rationale to direct research into new treatments.
In 1975, the National Cancer Institute (NCI) shifted its focus from relatively rare leukemias and lymphomas to solid tumors, which were much more common and did not respond well to traditional chemotherapy. Dr. John Minna headed up a new intramural branch of the NCI at the Veterans Administration Medical Center in Washington, DC, tasked with developing treatments for lung cancer. The research team he assembled for this research included Adi Gazdar, Daniel Ihde, Mary Matthews, Martin Cohen, and me. It was during this time that I came to appreciate what has become the guiding principle of my career; namely, that it is necessary to understand the biology of a disease in order to treat it. Dr. Minna believed that the best way to understand the biological basis of cancer was to study tumor cells. Unfortunately, lung cancer cells cannot easily be removed from patients, so we began to systematically attempt to culture tumor cell lines from patients treated at the facility. These cell lines became the basis of the NCI human cell lines, and most were derived from lung cancer patients, although some came from other solid tumors as well. At that time, a few oncogenes were already known; however, it was soon discovered that most of these tumor-derived cell lines, especially those from small cell lung cancer, were missing pieces of chromosomes. This, in turn, led to the discovery of tumor suppressor genes such as p53 and Rb, which are located in those missing pieces of genetic material. While these biologic studies were underway, clinical trials using chemotherapy demonstrated that many small cell lung cancer patients could be cured with a combination of chemotherapy and radiation therapy, and the combinations of agents could prolong survival in patients with advanced small cell lung cancer. The development of effective chemotherapy for non-small cell lung cancers lagged behind the developments in small cell lung cancer, and platinum doublets had lower response rates. Nonetheless, these platinum doublets made small improvements in the cure rates in early stages and some survival benefits in advanced stages.
Our research into lung cancer cell lines also revealed that non-small cell lung cancer tumor cells frequently secreted epidermal growth factor (EGF) and overexpressed EGF receptors (EGFRs). This discovery led to a number of new treatments based on attacking either the growth factor or the receptor such as the monoclonal antibody cetuximab originally developed by Drs. John Mendelsohn and Gordon Sato; these were among the first targeted therapies. Originally, targeted therapies were given to all patients without testing for the presence of appropriate targets, which resulted in only 10% of all patients responding to these antibodies. Several studies indicated that assessment of EGFR expression by IHC or FISH might predict superior benefit in high expressing patients.
Studies from our SPORE in Colorado showed that overexpression of EGFR, squamous angiogenic dysplasia, and overexpression of PGE2 developed in the dysplastic bronchial epithelium during the early carcinogenic process. Prostacyclin overexpression could prevent lung cancer development in animal models. Serial assessment of dysplastic changes by bronchoscopy could identify changes that associate with chemoprevention in former smokers leading to the possibility of preventing lung cancers by smoking cessation and by chemoprevention.
Another form of anti-EGFR therapy was the discovery of small molecule tyrosine kinase inhibitors (TKIs) that could bind to the EGFR ATP binding pocket. Early studies showed dramatic response in patients who did respond; the magnitude of those responses was dramatic due to activating mutations in their EGFRs as demonstrated by Drs. Bruce E. Johnson, Thomas J. Lynch, and others in 2004. The finding that EGFR TKIs were most effective in EGFR mutant tumors and that such therapy was superior to initial chemotherapy inaugurated the molecular treatment era for lung cancer that has now been expanded to many other oncogenic drivers. Additionally, while these therapies do not cure patients, subsequent studies have identified many of the causes of resistance and novel secondand third-generation TKIs are providing additional benefit in these patients. This finding once again illustrates the importance of using the underlying biology, in this case the presence or absence of EGFR mutations, to direct the appropriate course of treatment.
More recently, there have been successes in lung cancer treatment using inhibitors that target immune checkpoint proteins such as programmed cell death-1 (PD-1) and its ligand, PD-L1. These immunotherapies have been successful in producing extremely durable responses in some patients. Unlike molecular therapies, these immunotherapies may be able to produce complete responses (cures), though this remains to be seen. Like the molecular therapies, verifying the presence of the target, in this case PD-L1, improves the chances of getting a response, although better biomarkers are needed.
The push to find a cure for cancer has received renewed attention since President Obama called for a “National Cancer Moonshot” to eliminate cancer in his 2016 State of the Union Address. Many people are wondering if this effort can be successful, but that depends on how you define success. If you would consider the Moonshot successful if it contributes additional resources that will move research forward and improve care for patients in the long term, then the effort will likely be successful. However, if you would only consider the Moonshot a success if it produces a cure for cancer by 2020, you might be disappointed.
It is a great honor for me to win the Karnofsky award, but obviously many fabulous investigators conducted the work required for these advances. I consider this award as honoring all those investigators and patient volunteers who have contributed to these improvements in lung cancer outcomes. ✦
The ILCN congratulates Dr. Bunn on his receipt of this prestigious honor. He has been a major leader in the field of thoracic oncology, a scientific visionary with a practical clinical background. His work has helped advance the field and has contributed to cures in thousands of individuals affected with lung cancer. —Corey J. Langer, MD, Editor