By Gerard A. Silvestri, MD, MS, FCCP
A recent population-based study suggested the incidence of pulmonary nodules detected by CT is around 1.5 million per year. This finding is no surprise given the increasing use of chest CT for myriad of medical conditions and may increase even further as lung cancer screening is implemented nationally. The evaluation of pulmonary nodules is important because identifying malignant nodules should be performed as rapidly as possible while avoiding unnecessary and invasive testing for benign lesions. There are essentially 3 options for patients with pulmonary nodules, serial imaging, biopsy or PET scan, or surgical resection. The choice of the most appropriate option is based on the clinician’s pretest probability that the nodule is malignant. For a calculated pretest probability of cancer of less than 5%, serial imaging would be the preferred strategy. For nodules with a probability of cancer between 5% and 65%, PET scan or needle biopsy is indicated. Those with a high pretest probability of cancer (>65%) should be referred for surgical resection.
The evaluation of pulmonary nodules is important because identifying malignant nodules should be performed as rapidly as possible while avoiding unnecessary and invasive testing for benign lesions.
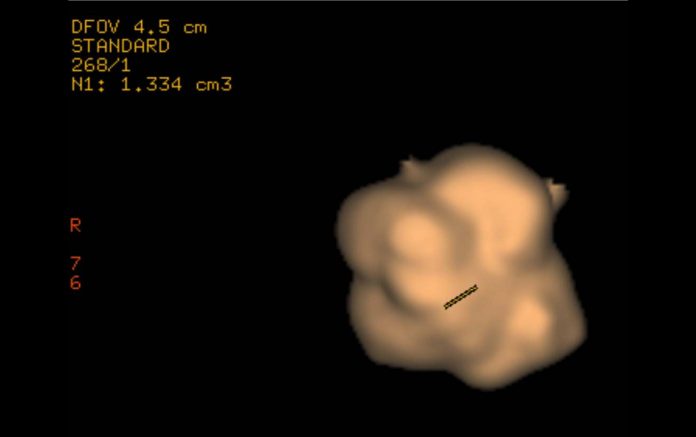
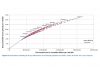
Several models are available for calculating the pretest probability of cancer in a pulmonary nodule. One model relies on 3 patient and 3 radiographic characteristics to stratify risk; where age, smoking history, and a history of extrathoracic malignancy are the patient factors, and edge characteristics of the nodule, upper lobe location, and size are the radiographic factors. Thus, an elderly smoker with a large, spiculated, upper lobe nodule has a much higher likelihood of cancer than a young, never smoking patient with a small, well circumscribed lower lobe nodule. McWilliams et al, extended this model to a population of patients with screen detected nodules. They confirmed the previous risk factors but also discovered patients with multiple pulmonary nodules are less likely to be diagnosed with cancer in the nodule in question. Other models incorporate PET findings when they are available. In addition, the findings of a completely calcified pulmonary nodule or the absence of growth over a 2-year period confirm benignity.
Once the pretest probability of cancer is calculated, clinicians should consider the advantages and disadvantages of each option. For nodules that have a low pretest probability of cancer, serial imaging for 2 years with chest CT is recommended. It has the advantage of being the least invasive option. Growth at any point during surveillance should lead to further testing with either biopsy or surgical resection. Both the American College of Chest Physicians (ACCP) and the Fleischner Society have provided guidance as to how often and for how long pulmonary nodules should be surveilled. In general, the larger the nodule or the higher the risk of cancer, the shorter the time interval between scans. The only downside of serial imaging is that a malignant nodule has the potential to grow between scans, though the penalty for missing tumor growth is unclear and must be weighed against invasive testing with its potential complications. For intermediate risk nodules, the choices are either PET scan or CT-guided transthoracic needle biopsy. PET scan has a relatively high sensitivity and specificity. However, both false positive and negative PET scans occur and clinicians should interpret the findings with caution. Focal pneumonia, granulomatous disease, among other entities can show uptake on PET and can cause clinicians to proceed with invasive testing when malignancy is not present. Conversely, false-negative PET scans occur, particularly in slow-growing malignancies such as adenocarcinoma in situ and carcinoid. In patients referred for surgery with a high pretest probability of cancer, a PET scan for staging the mediastinum and to search for metastatic disease is appropriate. Transthoracic needle aspiration can help avoid unnecessary surgery in cases where a benign diagnosis is considered. The accuracy is high. However, the tradeoff is an associated 15% pneumothorax rate, with 6% of patients requiring chest tube drainage. If there is a high degree of suspicion for cancer, a needle biopsy is not warranted because a negative biopsy will not be trusted, and the patient will be referred for surgery anyway.
While all three diagnostic approaches are valid in differing scenarios, patient preferences should be incorporated into the final decision. For example, a patient with low probability of cancer may insist the lesion be removed because of the anxiety associated with waiting between interval scans with the possibility that a cancer is growing.
In summary, a clinician’s suspicion of the probability that a nodule is cancer guides all further testing. As the probability of malignancy rises, the need for invasive testing increases. Future work is likely to incorporate radiographic volumetric measurements of the nodule to assess growth between serial images and biomarker assessment (either bronchoscopic or blood) that will help differentiate benignity from malignancy by less invasive means. ✦
References
Gould MK, Ananth L, Barnett PG. Veterans Affairs SNAP Cooperative Study Group. A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest. 2007;131:383-388.
Gould MK, Donington J, Lynch WR, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5_suppl):e93S-120S.
Gould MK, Tang T, Liu IL, et al. Recent trends in the identification of incidental pulmonary nodules. Am J Resp Crit Care Med. 2015;192: 1208-1214.
MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237:395-400.
McWilliams A, Tammemagi MC, Mayo JR, et al. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369:910-919.
Silvestri GA, Vachani, A, Whitney D, et al. A Bronchial Genomic Classifier for the Diagnostic Evaluation of Lung Cancer. N Engl J Med. 2015;373: 243-251.
Swensen SJ, Silverstein MD, Ilstrup DM, et al. The probability of malignancy in solitary pulmonary nodules. Application to small radiologically indeterminate nodules. Arch Intern Med. 1997;157:849-855.
van Klaveren RJ, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med. 2009;361:2221-2229.