By Emily Stone, MBBS, MMed, FRACP, and Graham Warren, MD, PhD
Tobacco control is set to become one of the most clinically effective and rapidly developing areas in lung cancer medicine. Since the original publication of the US Surgeon General’s Report (SGR) on Smoking and Health in 1964, the 2014 SGR report details the most current advances and observations: 1) tobacco use causes a wide spectrum of diseases, 2) tobacco cessation at any age results in significant health benefits, 3) smoking by cancer patients and survivors causes adverse cancer treatment outcomes, and 4) continued tobacco consumption will cause substantial financial and healthrelated economic costs worldwide.1 To prevent these effects, tobacco control measures must reduce smoking rates.
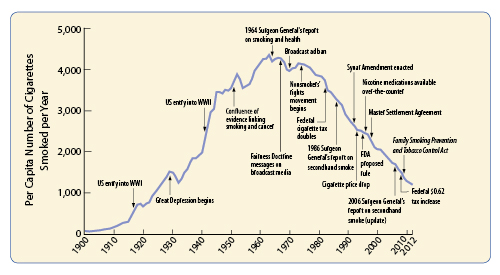
The link between smoking and lung cancer cannot be refuted. Starting with large pivotal studies that linked higher rates of lung cancer in people with higher rates of smoking,2,3 data are now conclusive that smoking causes 80%-90% of all lung cancer. The concomitant rise in tobacco consumption has turned lung cancer from a rare disease with several hundred cases annually in 1900 to several hundred thousand cases currently. Patterns have emerged worldwide. In high-income countries, the lung cancer epidemic is showing the effects of strong tobacco control, with peak lung-cancer incidence rates in men occurring around 1980,4 a couple of decades after the first US Surgeon General’s Report. Between 1964 and 1980, these countries witnessed the institution of multiple tobacco control measures and a subsequent decline in smoking in men. In many countries, we have yet to see stabilization or decline in lung cancer rates in women. Product design, including the introduction of filtered cigarettes and menthol over the past 50 years, has not reduced the harms of tobacco consumption and, in fact, has resulted in a more severe addiction.5
The benefits of smoking cessation are particularly relevant to lung cancer screening and cancer treatment. The National Lung Screening Trial study originally showed a 20% reduction in mortality for patients who received CT screening. 6 Impressively, follow-up analysis of the same trial demonstrated substantial reductions in mortality for patients who quit smoking, benefits that matched those of CT screening for patients who quit smoking for 7 years.7 Smoking cessation reduced mortality by 45% in a cohort of lung cancer patients who received phonebased cessation support.8 The benefits of smoking cessation after diagnosis have also been shown in patients treated with stereotactic body radiotherapy.9 Several studies highlighted in the 2014 SGR delineate the benefits of smoking cessation.1 The National Comprehensive Cancer Network (NCCN) has recently developed structured guidelines for smoking cessation in all cancer patients.10 Smoking cessation in patients with known or suspected lung cancer is an essential part of lung cancer treatment.
U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. Atlanta,
GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and
Health Promotion, Office on Smoking and Health, 2014
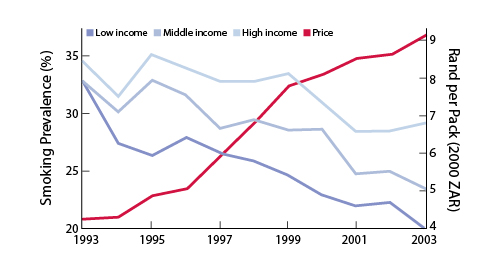
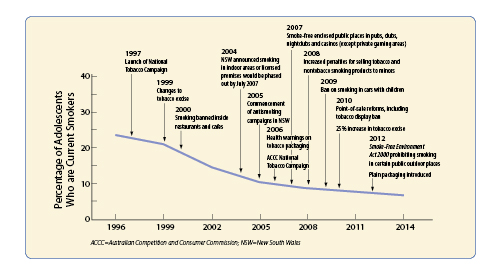
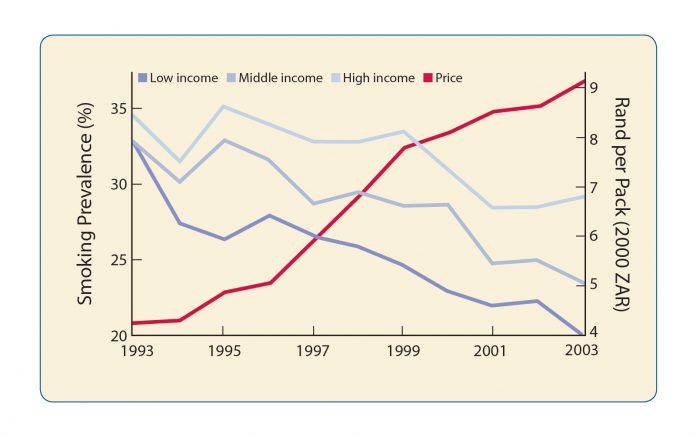
As clinicians, we often discuss smoking cessation with our patients, but we may less commonly consider the effect of population-based strategies. Tobacco control strategies have dramatically reduced smoking rates and improved health outcomes in countries that have implemented them. Clinicians can act as leaders to assist in local, regional, and national tobacco control efforts. The cornerstone of international tobacco control is the WHO Framework Convention on Tobacco Control and its MPOWER measures. The most effective strategies focus on tobacco taxation and cigarette price, smoking bans, and advertising bans including plain packaging. The many examples of such strategies are outside the scope of this brief article, but the accompanying figures demonstrate their effects on tobacco consumption in the US (Figure 1), in South Africa (Figure 2), and on adolescent smoking rates in Australia (Figure 3). Unfortunately, adverse governmental influence can severely impair tobacco control efforts. In China, the tobacco industry is a state-owned monopoly regulated (and promoted) at the highest government level, with power over the introduction of tobacco control measures due to its structural integration into the government bodies that oversee both tobacco industry growth and tobacco control. In Poland, recent efforts by tobacco industry representatives have influenced the content of tobacco control legislation. In the Netherlands, weakening of tobacco control legislation over recent years has raised concern about links between senior government members and the tobacco industry. The global tobacco industry is a critical driver of the current and future lung cancer epidemic. Opposing this are groups in all countries working actively to curb the adverse effects of tobacco. When promoting tobacco cessation in cancer care, clinicians should consider the tobacco control context in which they work and promote tobacco control efforts that benefit their patients and their own society.
Key Message Box
• Smoking cessation reduces the risk of lung cancer and of overall cause mortality in smokers, with up to 10 years of life saved in young smokers who quit
• Smoking cessation in lung cancer patients improves outcomes, including after treatment • Smoking cessation may be enhanced by lung cancer screening
• Tobacco control strategies are highly successful in reducing smoking rates and improving cessation wherever they are effectively applied
• The tobacco industry actively opposes tobacco control, interfering with government policy and pursuing new markets in vulnerable populations
References
1. Alberg AJ, Shopland DR, Cummings KM. The 2014 Surgeon General’s Report: Commemorating the 50th Anniversary of the 1964 Report of the Advisory Committee to the US Surgeon General and Updating the Evidence on the Health Consequences of Cigarette Smoking. Am J Epidemiol. 2014; 179:403–12.
2. Wynder EL, Graham EA. Tobacco smoking as a possible etiologic factor in bronchiogenic carcinoma; a study of 684 proved cases. J Am Med Assoc. 1950;143:329–36.
3. Doll R, Hill AB. Smoking and carcinoma of the lung; preliminary report. Br Med J. 1950; 2:739–48.
4. Islami F, Torre LA, Jemal A. Global trends of lung cancer mortality and smoking prevalence. Transl Lung Cancer Res. 2015; 4:327–38.
5. Thun MJ, Carter BD, Feskanich D, et al. 50-Year Trends in Smoking-Related Mortality in the United States. N Engl J Med. 2013; 368:351–64.
6. National Lung Screening Trial Research Team, Church TR, Black WC, et al. Results of initial low-dose computed tomographic screening for lung cancer. N Engl J Med. 2013; 368:1980–91.
7. Tanner NT, Kanodra NM, Gebregziabher M, et al. The Association Between Smoking Abstinence and Mortality in the National Lung Screening Trial. Am J Respir Crit Care Med. 2015; Available from: http://www.atsjournals.org/doi/abs/10.1164/rccm.201507-1420OC.
8. Dobson Amato KA, Hyland A, Reed R, et al. Tobacco Cessation May Improve Lung Cancer Patient Survival. JTO. 2015; 10:1014–9.
9. Roach MC, Rehman S, DeWees TA, Abraham CD, Bradley JD, Robinson CG. It’s never too late: Smoking cessation after stereotactic body radiation therapy for non-small cell lung carcinoma improves overall survival. Pract Radiat Oncol. 2016; 6:12-8.
10. NCCN Clinical Practice Guidelines in Oncology, Smoking Cessation. 2015. Available from: http://www.nccn.org/professionals/physician_gls/pdf/smoking.pdf.